Keeping Kidneys Safe: Smart Choices about Medicines
On this page:
- Manage your medicines with help from your health care providers
- Be careful about using over-the-counter medicines
- Plan ahead to manage pain, flu, or other illness
- Watch a video explaining why it’s important to plan ahead for illness and how NSAIDs can harm your kidneys
- If blood pressure medicines help my kidneys, why all this extra caution?
If you have chronic kidney disease (CKD), diabetes, or high blood pressure—or if you take certain blood pressure medicines that affect your kidneys—you should take steps to protect your kidneys from harm.
ACE inhibitors and ARBs are two types of blood pressure medicine that may slow the loss of kidney function and delay kidney failure. You can tell if you’re taking one of these medicines by its generic name. ACE inhibitors end in –pril and ARBs have generic names that end in –sartan; for example, lisinopril NIH external link and losartan NIH external link.
You may also take a diuretic, sometimes called a water pill, to meet your blood pressure goals.
The information below explains
- actions you can take to keep your kidneys safe while taking these blood pressure medicines
- why you sometimes need to take special care with medicines; for example, when you’re sick, dehydrated, or thinking about whether or not to take an over-the-counter (OTC) medicine

Manage your medicines with help from your health care providers
At the pharmacy
The next time you pick up a prescription or buy an OTC medicine or supplement, ask your pharmacist how the product may affect your kidneys or react with other medicines you take.
Fill your prescriptions at only one pharmacy or pharmacy chain so your pharmacist can monitor your medicines and supplements, and check for harmful interactions between your medicines.
At your doctor’s office
Keep an up-to-date list of your medicines and supplements in your wallet. Take your list with you, or bring all your medicine bottles, to all health care visits.

Be careful about using over-the-counter medicines
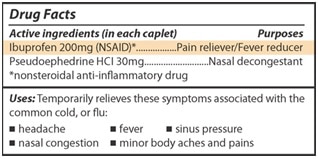
If you take OTC or prescription medicines for headaches, pain, fever, or colds, you may be taking a nonsteroidal anti-inflammatory drug (NSAID). NSAIDs include popular pain relievers and cold medicines that can damage your kidneys if you take them for a long time, or lead to acute kidney injury if you take them when you are dehydrated or your blood pressure is low.
Ibuprofen NIH external link and naproxen NIH external link are NSAIDs. NSAIDs are sold under many different brand names, so ask your pharmacist or health care provider if the medicines you take are safe to use.
You also can look for NSAIDs on Drug Facts labels like the one below.
Plan ahead to manage pain, flu, or other illness
Almost everyone gets sick once in a while. Your doctor or pharmacist can help you plan ahead to keep your kidneys safe until you get well. Prepare in advance so you know what to do if you have pain or a fever, diarrhea, nausea, or vomiting, which can lead to dehydration.
Before you get sick, ask your health care provider or pharmacist the following questions
- If I get sick, are there medicines I should not take while I’m sick?
- If I need to stop medicines when I’m sick, when can I restart them?
- What can I take or do to relieve a headache or other pain?
- What can I take to relieve a fever?
- If I have diarrhea or am vomiting, do I need to change how or when I take my blood pressure medicine?
Watch a video explaining why it’s important to plan ahead for illness and how NSAIDs can harm your kidneys
Discuss this video with your doctor, nurse, or pharmacist before you make any changes to the way you take your medicines.
If blood pressure medicines help my kidneys, why all this extra caution?
In normal, everyday circumstances, taking your blood pressure medicines as prescribed helps protect your kidneys. However, certain situations, such as when you’re dehydrated from the flu or diarrhea, can lower the blood flow to your kidneys and cause harm.
Factors that can add up to cause harm
When you get sick from something like the flu or diarrhea, or have trouble drinking enough fluids, the blood pressure in your body may decrease. As a result, the pressure in your kidneys can be low, too.
In most cases, healthy kidneys can protect themselves. However, if you keep taking your blood pressure medicines when you’re dehydrated or have low blood pressure, your kidneys might have a hard time protecting themselves. The pressure within your kidneys might drop so low that your kidneys won’t filter normally.
If you’re dehydrated, NSAIDs can also keep your kidneys from protecting themselves. As a result, taking NSAIDs when you’re sick and dehydrated can cause kidney injury.
Other ways to protect your kidneys
Read about what else you can do to keep your kidneys healthy. If you already have CKD, the steps you take to protect your kidneys also may help prevent heart disease—and improve your health overall.
Clinical Trials
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and other components of the National Institutes of Health (NIH) conduct and support research into many diseases and conditions.
What are clinical trials, and are they right for you?
Clinical trials are part of clinical research and at the heart of all medical advances. Clinical trials look at new ways to prevent, detect, or treat disease. Researchers also use clinical trials to look at other aspects of care, such as improving the quality of life for people with chronic illnesses. Find out if clinical trials are right for you NIH external link.
What clinical trials are open?
Clinical trials that are currently open and are recruiting can be viewed at ClinicalTrials.gov NIH external link.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
The NIDDK would like to thank Jeffrey Fink, MD, MS, Chief, Division of General Internal Medicine, University of Maryland School of Medicine

