What is urodynamic testing?
Urodynamic testing is any procedure that looks at how well parts of the lower urinary tract—the bladder, sphincters, and urethra—work to store and release urine. Most urodynamic tests focus on how well your bladder can hold and empty urine. Urodynamic tests can also show whether your bladder is contracting when it’s not supposed to, causing urine to leak.
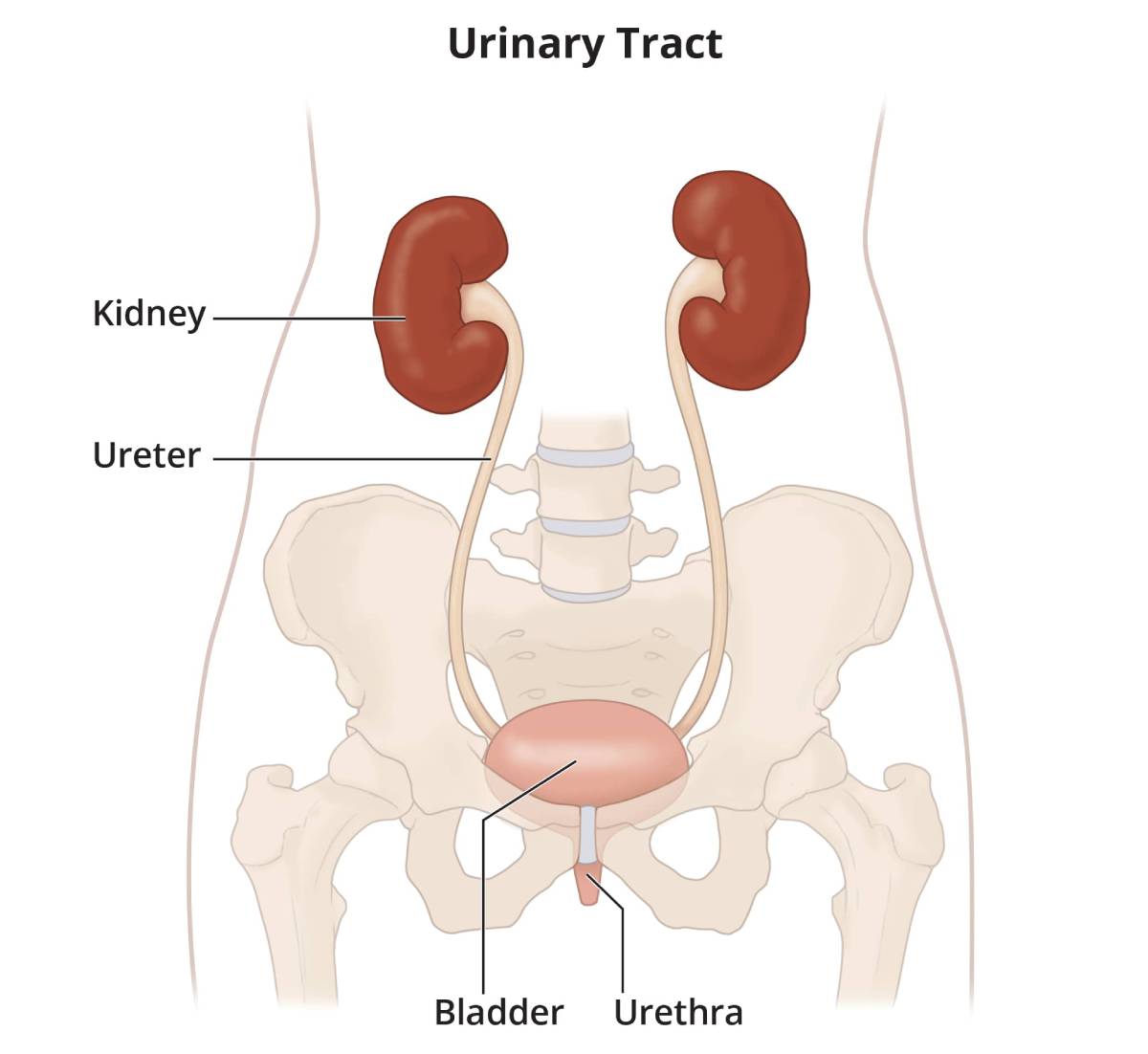 All parts of the urinary tract—the kidneys, ureters, bladder, and urethra—must work together to urinate normally.
All parts of the urinary tract—the kidneys, ureters, bladder, and urethra—must work together to urinate normally.
Why do health care professionals use urodynamic tests?
Urodynamic tests are used to determine if there are problems with your lower urinary tract. Testing may be recommended if you
- leak urine
- go to the bathroom frequently
- feel pain while urinating
- feel a sudden, strong urge to use the bathroom
- have trouble starting to urinate
- have problems emptying your bladder completely
- have repeated urinary tract infections
What urodynamic tests do health care professionals use?
Health care professional may use the following tests
- uroflowmetry
- postvoid residual urine measurement
- cystometric test
- leak point pressure measurement
- pressure flow study
- electromyography
- video urodynamic tests
Uroflowmetry
Uroflowmetry measures how much urine is in your bladder and how fast the urine comes out, also known as flow rate. The results of this test can show if your bladder muscles are weak or if urine flow is blocked.
During a uroflowmetry test, you urinate into a special toilet or funnel that has two parts: a container for collecting the urine and a scale. The uroflowmetry equipment creates a graph that shows changes in the flow rate while you urinate. Your health care professional uses the graph to see when the flow rate is the highest and how many seconds it takes to get there.
Your flow rate can also be measured by recording how long it takes to urinate into a special container that accurately measures how much urine you release.

Postvoid residual measurement
This urodynamic test measures how much urine is left in your bladder after you urinate. If you have 100–150 milliliters of urine or more left in your bladder, your bladder is not emptying completely. This test can be conducted with an ultrasound or by feeding a catheter into your bladder to drain and measure remaining urine.
Bladder ultrasounds are performed by a specially trained technician in a health care professional’s office, radiology center, or hospital.
Cystometric test
A cystometric test measures
- how much urine your bladder can hold
- how much pressure builds up inside your bladder as it stores urine
- how full your bladder is when you start feeling the urge to urinate
First, a catheter is used to empty your bladder completely. Then a special, smaller catheter is placed in the bladder. This catheter has a pressure-measuring device called a manometer. Another catheter may be placed in the rectum or vagina to record pressure there.
Once you completely empty your bladder, it is filled slowly with warm water. You’ll be asked to describe how the bladder feels and when you feel the need to start urinating. When you start feeling that urge, the volume of water and the bladder pressure are recorded.
You may be asked to cough or strain during this procedure to see if the bladder pressure changes or if you leak urine.
A cystometric test can also identify if your bladder contracts when it’s not supposed to.

While you’re having a cystometric test or right afterward, your health care professional might decide to do a leak point pressure measurement or a pressure flow study.
Leak point pressure measurement
While your bladder is being filled with warm water for the cystometric test, it may suddenly contract and squeeze some water out without warning. A manometer measures the pressure inside your bladder when this leakage occurs, identifying the leak point pressure. This information can tell your health care professional more about the kind of bladder problem you have.
You may be asked to cough, shift position, or try to exhale while holding your nose and mouth. These actions help your health care professional evaluate the sphincters that help keep your urine in.
Pressure flow study
A pressure flow study measures how much pressure your bladder needs to urinate and how quickly your urine flows at that pressure. After the cystometric test, you will be asked to empty your bladder while a manometer measures your bladder pressure and flow rate.
A pressure flow study can help identify any bladder outlet blockage that may be caused by prostate enlargement; an anterior vaginal wall prolapse, also known as a cystocele; or urinary incontinence correction surgery.
Electromyography
A health care professional may recommend a electromyography if your urinary problem is likely related to nerve or muscle damage.
Electromyography uses special sensors to measure the electrical activity of the muscles and nerves in and around your bladder and sphincters. The sensors are placed on your skin near the urethra and rectum or on a urethral or rectal catheter. Muscle and nerve activity is recorded on a machine. The patterns of the nerve impulses show whether the messages sent to your bladder and pelvic floor muscles are coordinating correctly.
A numbing gel is used to reduce discomfort if the sensors are on a catheter rather than on your skin.
Video urodynamic tests
Video urodynamic tests use x-rays or ultrasound to take pictures and videos of your bladder while it fills and empties. A trained technician may use a catheter to fill your bladder with contrast or dye for a better picture.
How do I prepare for a urodynamic test?
Most urodynamic tests don’t involve special preparations. You might be asked to change your fluid intake or stop taking certain medicines. You may also be instructed to arrive for testing with a full bladder.
What should I expect after a urodynamic test?
After having urodynamic tests, you may feel mild discomfort for a few hours when urinating. Drinking an 8-ounce glass of water every half-hour for 2 hours may help to reduce discomfort. Your health care professional
- may recommend taking a warm bath or holding a warm, damp washcloth over the urethral opening to relieve discomfort
- might prescribe an antibiotic to prevent infection
If you show any signs of infection—including pain, chills, or fever—call your health care professional immediately.
Results for simple tests such as cystometry and uroflowmetry are often available immediately after the test.
Results of other tests, such as electromyography and video urodynamic tests, may take a few days to come back.
Your health care professional will talk with you about the results and possible treatments.
What are the risks of urodynamic tests?
Most urodynamic tests have no risk of complications. If you had a catheter inserted into your bladder, you may have a slight risk of developing a bladder infection (UTI).