Preventing Diabetes Problems
- Diabetes, Heart Disease, & Stroke
- Low Blood Glucose (Hypoglycemia)
- Diabetic Neuropathy
- Diabetic Kidney Disease
- Diabetes & Foot Problems
- Diabetic Eye Disease
- Diabetes, Gum Disease, & Other Dental Problems
- Diabetes, Sexual, & Bladder Problems
Diabetes, Heart Disease, & Stroke
On this page:
- What is the link between diabetes, heart disease, and stroke?
- What else increases my chances of heart disease or stroke if I have diabetes?
- How can I lower my chances of a heart attack or stroke if I have diabetes?
- How do doctors diagnose heart disease in people with diabetes?
- What are the warning signs of heart attack and stroke?
- Clinical Trials for Diabetes, Heart Disease, & Stroke
Having diabetes means you are more likely to develop heart disease. People with diabetes are also more likely to have certain risk factors, such as high blood pressure or high cholesterol, that increase their chances of having a heart attack or a stroke.
If you have diabetes, you can protect your heart and health by managing your blood glucose, also called blood sugar. You can also protect yourself by controlling your high blood pressure and high cholesterol. If you smoke, get help to stop.
What is the link between diabetes, heart disease, and stroke?
High blood glucose from diabetes can damage your blood vessels and the nerves that control your heart and blood vessels. Over time, this damage can lead to heart disease.1
People with diabetes tend to develop heart disease at a younger age than people without diabetes. Adults with diabetes are nearly twice as likely to have heart disease or stroke as adults without diabetes.2,3
The good news is that the steps you take to manage your diabetes also help lower your chances of having heart disease or stroke.
What else increases my chances of heart disease or stroke if I have diabetes?
Your risk for heart disease is greater if you are male rather than female, whether you have diabetes or not.2 If you do have diabetes, other factors add to your chances of developing heart disease or having a stroke.
Smoking
Smoking raises your risk of developing heart disease. If you have diabetes, it is important to stop smoking, because both smoking and diabetes narrow blood vessels. Smoking also increases your chances of developing other long-term problems such as
- lung disease
- lower leg infections and ulcers
- foot or leg amputation
High blood pressure
If you have high blood pressure, your heart works harder to pump blood. High blood pressure can strain your heart, damage blood vessels, and increase your risk of heart attack, stroke, and eye or kidney problems. Have your blood pressure checked regularly and work with your doctor to control or lower high blood pressure.
Abnormal cholesterol levels
Cholesterol is a type of fat, produced by your liver and found in your blood. You have two kinds of cholesterol in your blood: LDL and HDL.
LDL, often called “bad” cholesterol, can build up and clog your blood vessels. High levels of LDL cholesterol raise your risk of developing heart disease. HDL is sometimes called “good cholesterol.” Higher levels of HDL is linked to lower risk for heart disease and stroke. To improve LDL and HDL levels, limit the amount of fat in your eating plan, eat more plant-based foods, and get regular physical activity.
Another type of blood fat, triglycerides, also can raise your risk of heart disease when the levels are higher than recommended by your health care team.
Obesity and belly fat
Being overweight or having obesity can make it harder to manage your diabetes and raise your risk for many health problems, including heart disease and high blood pressure. If you are overweight, a healthy eating plan with fewer calories and more physical activity often will lower your blood glucose levels and reduce your need for medicines.
Excess belly fat around your waist, even if you are not overweight, can raise your chances of developing heart disease.
You have excess belly fat if your waist measures
- more than 40 inches and you are a man
- more than 35 inches and you are a woman
Chronic kidney disease
Heart disease is closely linked with chronic kidney disease, a condition in which your kidneys are damaged and can’t filter blood the way they should. Having diabetes is a risk factor for developing kidney disease, which affects about 40% of people with diabetes. Other risk factors for developing kidney disease are high blood pressure and a family history of kidney failure.
If you have risk factors, get tested for kidney disease and protect your kidneys by making healthy food choices, being more active, aiming for a healthy weight, and managing health conditions that cause kidney damage.
Family history of heart disease
A family history of heart disease may add to your chances of developing the condition. If one or more of your family members had a heart attack before age 50, you have double the chance of developing heart disease compared with people who have no family history of the disease.4
You can’t change whether heart disease runs in your family. But if you have diabetes, it’s even more important to take steps to protect yourself from heart disease and decrease your chances of having a stroke.
How can I lower my chances of a heart attack or stroke if I have diabetes?
Taking care of your diabetes is important to help you protect your heart. You can substantially lower your chances of having a heart attack or stroke by taking the following steps to keep your heart and blood vessels healthy.5
Manage your diabetes ABCs
Know your diabetes ABCs to help you manage your blood glucose, blood pressure, and cholesterol. Stop smoking if you have diabetes to lower your chances of developing heart disease.
A is for the A1C test
The A1C test shows your average blood glucose level over the past 3 months. This is different from the blood glucose checks you do every day. The higher your A1C number, the higher your blood glucose levels have been during the past 3 months. High levels of blood glucose can harm your heart, blood vessels, kidneys, feet, and eyes.
The A1C goal for many people with diabetes is below 7%. Some people may do better with a slightly higher A1C goal. Your A1C goals may also change as you get older and your lifestyle changes. Ask your health care team what your goal should be.
B is for blood pressure
Blood pressure is the force of your blood against the wall of your blood vessels. If your blood pressure gets too high, it makes your heart work too hard. High blood pressure can cause a heart attack or stroke and damage your kidneys and eyes.
The blood pressure goal for most people with diabetes is below 140/90 mm Hg. Ask what your goal should be.
C is for cholesterol
A buildup of cholesterol, a form of fat found in your blood, can cause a heart attack or stroke. Ask your health care team what your cholesterol numbers should be. If you are over 40 years old, you may need to take medicine, such as a statin, to lower your cholesterol levels and protect your heart. Some people with very high LDL (“bad”) cholesterol may need to take medicine starting at a younger age.
Learn about getting your cholesterol checked.
S is for stop smoking
Quitting smoking is especially important for people with diabetes because both smoking and diabetes narrow blood vessels, so your heart has to work harder. E-cigarettes aren’t a safe option either.
If you quit smoking
- you will lower your risk for heart attack; stroke; nerve, kidney, and eye disease; and amputation
- your blood glucose, blood pressure, and cholesterol levels may improve
- your blood circulation will improve
- you may have an easier time being physically active
If you smoke or use other tobacco products, stop. Ask for help so you don’t have to do it alone. You can start by calling the National Quitline at 1-800-QUITNOW or 1-800-784-8669. For tips on quitting, go to Smokefree.gov.
Ask your health care team about your goals for A1C, blood pressure, and cholesterol, and what you can do to reach these goals. To improve your diabetes self-management skills, you may want a referral to a diabetes educator or a registered dietitian. Medicare, some private insurers, and other organizations will provide financial assistance for some of these services.
You can keep track of your ABCs with a diabetes record form. You can use it when you meet with your health care team in person or remotely. Talk with your team about your goals and how you are doing, and whether you need to make any changes to your diabetes care plan.
Develop or maintain healthy lifestyle habits
 Develop or maintain healthy lifestyle habits. Physical activity can help you manage your diabetes and may help you cope with stress.
Develop or maintain healthy lifestyle habits. Physical activity can help you manage your diabetes and may help you cope with stress.Healthy lifestyle habits that you stick with can help you manage your diabetes and prevent heart disease.
- Follow your healthy eating plan.
- Make physical activity part of your routine.
- Stay at or get to a healthy weight.
- Get enough sleep.
Learn more about these tips to manage diabetes.
Watch a video about what you can do to keep your heart healthy.
Learn about the Body Weight Planner, which may help you create a personal plan to reach your goal weight.
Learn to manage stress
 Yoga and other forms of exercise can help reduce stress.
Yoga and other forms of exercise can help reduce stress.Managing diabetes is not always easy. Feeling stressed, sad, lonely, or angry is common when you are living with diabetes. You may know what to do to stay healthy but may have trouble sticking with your plan over time. Long-term stress can raise your blood glucose and blood pressure, but you can learn ways to lower your stress. Try deep breathing, gardening, taking a walk, doing yoga, talking with a loved one, working on a hobby, or listening to your favorite music. Learn more about healthy ways to cope with stress.
Take medicine to protect your heart
Medicines may be an important part of your treatment plan. Your doctor will prescribe medicine based on your specific needs. Medicine may help you
- meet your A1C (blood glucose), blood pressure, and cholesterol goals.
- reduce your risk of blood clots, heart attack, or stroke.
- treat angina, or chest pain that is often a symptom of heart disease. Angina can also be an early symptom of a heart attack.
- treat heart failure, which is a form of heart disease in which your heart cannot pump blood well enough for your body to work properly.
 Take medicines as prescribed.
Take medicines as prescribed.Ask your doctor whether you should take daily aspirin. Aspirin is not safe for everyone. Your doctor can tell you whether taking aspirin is right for you and exactly how much to take.
Statins can reduce the risk of having a heart attack or stroke in some people with diabetes. In addition, certain diabetes medicines have been shown to reduce the risk of heart attacks and death in patients at very high risk of having a heart attack. Talk with your doctor to find out whether taking a statin or a diabetes medicine that reduces heart attack risk is right for you.
Take medicines the way your doctor or health care team tells you to. Talk with your doctor or pharmacist if you have questions about your medicines. Before you start a new medicine, ask your doctor about possible side effects and how you can avoid them. If the side effects of your medicine bother you, tell your doctor. Don’t stop taking your medicines without checking with your doctor first.
How do doctors diagnose heart disease in people with diabetes?
Doctors diagnose heart disease in people with diabetes based on their
- symptoms
- medical and family history
- how likely they are to have heart disease
- a physical exam
- results from tests and procedures
Tests used to monitor your diabetes—A1C, blood pressure, and cholesterol—help your doctor decide whether it is important to do additional tests to check your heart health or to refer you to a specialist such as a cardiologist.
 Your health care professional will do a physical exam.
Your health care professional will do a physical exam.Ask your health care team these questions.
- What can we do to lower my chances of getting heart disease?
- How can we work together to help me maintain my goals for A1C, blood pressure, and cholesterol?
- What medicines, such as aspirin or a statin, will help protect my heart?
- Are there diabetes medicines that will help protect my heart?
What are the warning signs of heart attack and stroke?
Call 9-1-1 right away if you have any of these warning signs of a heart attack
- pain or pressure in your chest that lasts longer than a few minutes or goes away and comes back
- pain or discomfort in one or both of your arms or shoulders, or your back, neck, or jaw
- shortness of breath
- sweating or light-headedness
- indigestion or nausea (feeling sick to your stomach)
- feeling very tired
Treatment works best when it is given right away. Warning signs can be different in different people. You may not have all the listed symptoms.
Women may experience chest pain, nausea, and vomiting; feel very tired (sometimes for days); and have pain that spreads to the back, neck, throat, arms, shoulders, or jaw. People with diabetes-related nerve damage may not notice any chest pain.
If you have angina, it’s important to know how and when to seek medical treatment.
 Call 9-1-1 if you have the warning signs of a heart attack or stroke. Treatment works best when given right away.
Call 9-1-1 if you have the warning signs of a heart attack or stroke. Treatment works best when given right away.Call 9-1-1 right away if you have any of these warning signs of a stroke, including sudden
- weakness or numbness of your face, arm, or leg on one side of your body
- confusion, or trouble talking or understanding
- dizziness, loss of balance, or trouble walking
- trouble seeing out of one or both eyes
- sudden, severe headache
If you have any one of these warning signs, call 9-1-1. You can help prevent permanent damage by getting to a hospital within an hour of a stroke.
Clinical Trials for Diabetes, Heart Disease, & Stroke
The NIDDK conducts and supports clinical trials in many diseases and conditions, including diabetes. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for diabetes, heart disease, and stroke?
Clinical trials—and other types of clinical studies—are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help doctors and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of diabetes, heart disease, and stroke, such as
- risk factors for heart disease and stroke in specific populations, such as Black Americans with diabetes
- improved imaging techniques and tests to help diagnose and treat conditions that lead to heart attacks and stroke
- the role of genetics in diabetes, heart disease, and stroke
Find out if clinical studies are right for you.
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical trials for heart disease and stroke are looking for participants?
You can view a filtered list of clinical studies on diabetes and heart disease that are federally funded, open, and recruiting at ClinicalTrials.gov. A separate list of clinical studies on diabetes and stroke is also available at ClinicalTrials.gov. You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe. Always talk with your health care provider before you participate in a clinical study.
References
Low Blood Glucose (Hypoglycemia)
On this page:
- What is low blood glucose?
- How common is low blood glucose?
- Who is more likely to develop low blood glucose?
- What are the symptoms of low blood glucose?
- What are the complications of low blood glucose?
- What causes low blood glucose in people with diabetes?
- How can I prevent low blood glucose if I have diabetes?
- How do I treat low blood glucose?
- What if I have severe low blood glucose and can’t treat myself?
- Clinical Trials for Low Blood Glucose
What is low blood glucose?
Low blood glucose, also called low blood sugar or hypoglycemia, occurs when the level of glucose in your blood drops below what is healthy for you. For many people with diabetes, this means a blood glucose reading lower than 70 milligrams per deciliter (mg/dL).1 Your number might be different, so check with your doctor or health care team to find out what blood glucose level is low for you.
How common is low blood glucose?
Low blood glucose is common among people with type 1 diabetes and among people with type 2 diabetes who take insulin or some other diabetes medicines. In a large global study of people with diabetes who take insulin, 4 in 5 people with type 1 diabetes and nearly half of those with type 2 diabetes reported a low blood sugar event at least once over a 4-week period.2
Severely low blood glucose, defined as when your blood glucose level drops so low you can’t treat it yourself, is less common. Among U.S. adults with diabetes who take insulin or some diabetes medicines that help the pancreas release insulin into the blood, 2 in 100 may develop severely low blood glucose each year.3
Who is more likely to develop low blood glucose?
You are more likely to develop low blood glucose if you4
- have type 1 diabetes
- take insulin or some other diabetes medicines
- are age 65 or older5
- had low blood glucose before
- have other health problems, such as kidney disease, heart disease, or cognitive impairment
What are the symptoms of low blood glucose?
Symptoms of low blood glucose tend to come on quickly and can vary from person to person. As Table 1 below shows, symptoms can range from mild to severe.
Table 1. Symptoms of low blood glucose6
| Mild-to-Moderate | Severe |
|---|---|
|
If your blood glucose level is low, you may feel
|
If your blood glucose level is very low, your brain may stop working as it should. You may
Severe hypoglycemia is dangerous and needs to be treated right away. |
Low blood glucose during sleep
Your blood glucose level can drop while you sleep and stay low for several hours, causing serious problems.7 Symptoms of low blood glucose while you sleep can include
- crying out or having nightmares
- sweating enough to make your pajamas or sheets damp
- feeling tired, irritable, or confused after waking up
Although you may not wake up or notice any symptoms, low blood glucose can interfere with your sleep, which may affect your quality of life, mood, and ability to work. Having low blood glucose during sleep can also make you less likely to notice and respond to symptoms of low blood glucose during the day.
What are the complications of low blood glucose?
Mild-to-moderate low blood glucose can be easily treated. But severely low blood glucose can cause serious complications, including passing out, coma, or death.
Repeated episodes of low blood glucose can lead to
- high blood glucose levels, if worry or fear of low blood glucose keeps you from taking the medicines you need to manage your diabetes8
- hypoglycemia unawareness, a condition in which you don’t notice any symptoms of low blood glucose until your blood glucose level has dropped very low
What causes low blood glucose in people with diabetes?
Low blood glucose levels can be a side effect of insulin or some other medicines that help your pancreas release insulin into your blood. Taking these can lower your blood glucose level.
 Insulin and some other diabetes medicines can lower your blood glucose level.
Insulin and some other diabetes medicines can lower your blood glucose level.Two types of diabetes pills can cause low blood glucose
- sulfonylureas, usually taken once or twice per day, which increase insulin over several hours
- meglitinides, taken before meals to promote a short-term increase in insulin
The following may also lower your blood glucose level
- Not eating or drinking enough carbohydrates (carbs). When you eat foods or drink beverages that contain carbohydrates, your digestive system breaks down the sugars and starches into glucose. Glucose then enters your bloodstream and raises your blood glucose level. If you don’t eat enough carbohydrates or skip or delay any meals, your blood glucose level could drop lower than what is healthy for you.
- Fasting. Continuing to take medicines that lower your glucose level while fasting for a medical procedure or for other purposes can also increase the risk for low blood glucose.
- Increasing physical activity. Increasing your physical activity level beyond your usual routine can lower your blood glucose level for up to 24 hours after the activity. Learn more about diabetes, eating, and physical activity.
- Drinking too much alcohol without enough food. Alcohol makes it harder for your body to keep your blood glucose level steady, especially if you haven’t eaten in a while. Alcohol can also keep you from feeling the first symptoms of low blood glucose, which can lead to severe symptoms.
- Being sick. When you’re sick, you may not be able to eat as much or keep food down, which can lower blood glucose.
How can I prevent low blood glucose if I have diabetes?
If you take insulin or other medicines that lower blood glucose, the following actions may help you prevent low blood glucose levels.
- Ask your doctor or health care team how to check your blood glucose level. The most common way to do so is by using a blood glucose meter. If you have hypoglycemia unawareness or have low blood glucose often, a continuous glucose monitor (CGM) may be a good option. The CGM measures your blood glucose level at regular times and can sound an alarm if it drops below your target range.
- Make sure your regular eating plan includes meals, snacks, and beverages with enough carbohydrates to help keep your blood glucose level in your target range. Carry a source of fast-acting carbohydrate, such as glucose tablets or a juice box, with you. Also, if you drink alcoholic beverages, it’s safer to eat some food at the same time.
- Be safe during exercise or physical activity. Physical activity can lower your blood glucose during the activity and for hours afterward. You may need to check your blood glucose before, during, and after physical activity and adjust your medicine or carbohydrate intake to prevent low blood glucose. For example, you might eat a snack before physical activity to prevent low blood glucose.
- Work with your doctor or health care team to prevent low blood glucose. Ask your team if any of your diabetes medicines can cause low blood glucose and how you can prevent and treat symptoms. Work with your doctor or health care team to adjust your diabetes management plan as needed.
 Some CGMs let you track your blood glucose levels using a small sensor attached to your arm or abdomen and view the information on your smartphone.
Some CGMs let you track your blood glucose levels using a small sensor attached to your arm or abdomen and view the information on your smartphone.How do I treat low blood glucose?
 If your blood glucose is below your target, take 15 to 20 grams of glucose or carbohydrates right away.
If your blood glucose is below your target, take 15 to 20 grams of glucose or carbohydrates right away.
If you begin to feel one or more symptoms of low blood glucose, check your blood glucose level. If your blood glucose level is below your target or less than 70 mg/dL, follow these steps
- Eat or drink 15 to 20 grams of glucose or carbohydrates right away. Examples include
- four glucose tablets or one tube of glucose gel.
- 1/2 cup (4 ounces) of fruit juice—not low-calorie or reduced-sugar juice. If you have kidney disease, don’t drink orange juice because it has a lot of potassium. Apple, grape, or cranberry juice are good options.
- 1/2 can (4 to 6 ounces) of soda—not low-calorie or reduced-sugar soda.
- 1 tablespoon of sugar, honey, or corn syrup.
- Wait 15 minutes and check your blood glucose level again. If your glucose level is still low, eat or drink another 15 to 20 grams of glucose or carbohydrates.
- Check your blood glucose level again after another 15 minutes. Repeat these steps until your glucose level is back to your target range.
- If your next meal is more than 1 hour away, have a snack to keep your blood glucose level within a range that is healthy for you. Try crackers or a piece of fruit.
Treating low blood glucose if you take medicines that slow down digestion
Some diabetes medicines slow down the digestion of carbohydrates to keep blood glucose levels from rising too high after you eat. If you develop low blood glucose while taking these medicines, you will need to take glucose tablets or glucose gel right away. Eating or drinking other sources of carbohydrates won’t raise your blood glucose level quickly enough.
What if I have severe low blood glucose and can’t treat myself?
Glucagon—a hormone that raises blood glucose levels—is the best way to treat severely low blood glucose. Available as an injection or a nasal spray, glucagon will quickly raise your blood glucose level. Your doctor can prescribe you a glucagon kit for use in case of an emergency.
If your blood glucose level drops very low, you won’t be able to treat it by yourself. Be prepared to address severely low blood glucose by
- talking with your doctor or health care team about when and how to use a glucagon emergency kit. If you have an emergency kit, regularly check the date on the package to make sure it hasn’t expired.
- teaching your family, friends, and coworkers when and how to give you glucagon. Tell them to call 911 right away after giving you glucagon or if you don’t have a glucagon emergency kit with you.
- wearing a medical alert identification bracelet or pendant. A medical alert ID tells other people that you have diabetes and need care right away. Getting prompt care can help prevent the serious problems that low blood glucose levels can cause.
Clinical Trials for Low Blood Glucose
The NIDDK conducts and supports clinical trials in many diseases and conditions, including diabetes. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for low blood glucose?
Clinical trials—and other types of clinical studies—are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help doctors and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of low blood glucose levels in diabetes, such as
- how to diagnose and treat low blood glucose among people with diabetes
- medicines that can treat symptoms of low blood glucose in people with hypoglycemia unawareness
- educational approaches to reduce fear of low blood glucose, which can make it harder for you to control your diabetes
Find out if clinical studies are right for you.
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical studies for low blood glucose are looking for participants?
You can view a filtered list of clinical studies on low blood glucose that are federally funded, open, and recruiting at ClinicalTrials.gov. You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe. Always talk with your health care provider before you participate in a clinical study.
References
Diabetic Neuropathy
Diabetic neuropathy is nerve damage that can occur in people with diabetes. Different types of nerve damage cause different symptoms. Symptoms can range from pain and numbness in your feet to problems with the functions of your internal organs, such as your heart and bladder.
What Is Diabetic Neuropathy?
Diabetic neuropathy is nerve damage that is caused by diabetes. Over time, high blood glucose levels, also called blood sugar, and high levels of fats, such as triglycerides, in the blood from diabetes can damage your nerves. Symptoms depend on which type of diabetic neuropathy you have.
Peripheral Neuropathy
Peripheral neuropathy is a type of nerve damage that typically affects the feet and legs and sometimes affects the hands and arms. This type of neuropathy is very common. About one-third to one-half of people with diabetes have peripheral neuropathy.
Autonomic Neuropathy
Autonomic neuropathy is damage to nerves that control your internal organs, leading to problems with your heart rate and blood pressure, digestive system, bladder, sex organs, sweat glands, and eyes. The damage can also lead to hypoglycemia unawareness.
Focal Neuropathies
Focal neuropathies are conditions in which you typically have damage to single nerves, most often in your hand, head, torso, or leg. The most common types of focal neuropathy are entrapment syndromes, such as carpal tunnel syndrome. Other types of focal neuropathy are much less common.
Proximal Neuropathy
Proximal neuropathy is a rare and disabling type of nerve damage in your hip, buttock, or thigh. The damage typically affects one side of your body and may rarely spread to the other side. Symptoms gradually improve over a period of months or years.
Clinical Trials
The NIDDK and other components of the National Institutes of Health (NIH) support and conduct research into many diseases and conditions. View clinical trials that are currently recruiting volunteers.
Related Conditions & Diseases
- Diabetes
- Diabetes and Foot Problems
- Erectile Dysfunction
- Gastroparesis
- Diabetes and Sexual and Urologic Problems
- Constipation
- Diarrhea
- Bowel Control Problems
Related Research
See more about diabetes research at the NIDDK.
Additional Languages
This content is also available in:
Diabetic Kidney Disease
In this section:
- What is diabetic kidney disease?
- How does diabetes cause kidney disease?
- What increases my chances of diabetic kidney disease?
- How can I tell if I have diabetic kidney disease?
- How can I keep my kidneys healthy if I have diabetes?
- How can I cope with the stress of managing my diabetes?
- Does diabetic kidney disease get worse over time?
What is diabetic kidney disease?
Diabetic kidney disease is a type of kidney disease caused by diabetes.
Diabetes is the leading cause of kidney disease. About 1 out of 3 adults with diabetes has kidney disease.1
The main job of the kidneys is to filter wastes and extra water out of your blood to make urine. Your kidneys also help control blood pressure and make hormones that your body needs to stay healthy.
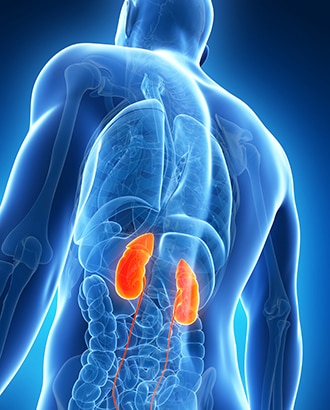
When your kidneys are damaged, they can’t filter blood like they should, which can cause wastes to build up in your body. Kidney damage can also cause other health problems.
Kidney damage caused by diabetes usually occurs slowly, over many years. You can take steps to protect your kidneys and to prevent or delay kidney damage.
Watch a video about diabetes and kidney disease.
What are other names for diabetic kidney disease?
Diabetic kidney disease is also called DKD, chronic kidney disease, CKD, kidney disease of diabetes, or diabetic nephropathy.
How does diabetes cause kidney disease?
High blood glucose, also called blood sugar, can damage the blood vessels in your kidneys. When the blood vessels are damaged, they don’t work as well. Many people with diabetes also develop high blood pressure, which can also damage your kidneys. Learn more about high blood pressure and kidney disease.
What increases my chances of developing diabetic kidney disease?
Having diabetes for a longer time increases the chances that you will have kidney damage. If you have diabetes, you are more likely to develop kidney disease if your
- blood glucose is too high
- blood pressure is too high
African Americans, American Indians, and Hispanics/Latinos develop diabetes, kidney disease, and kidney failure at a higher rate than Caucasians.
You are also more likely to develop kidney disease if you have diabetes and
- smoke
- don’t follow your diabetes eating plan
- eat foods high in salt
- are not active
- are overweight
- have heart disease
- have a family history of kidney failure

How can I tell if I have diabetic kidney disease?
Most people with diabetic kidney disease do not have symptoms. The only way to know if you have diabetic kidney disease is to get your kidneys checked.
Health care professionals use blood and urine tests to check for diabetic kidney disease. Your health care professional will check your urine for albumin and will also do a blood test to see how well your kidneys are filtering your blood.
You should get tested every year for kidney disease if you
- have type 2 diabetes
- have had type 1 diabetes for more than 5 years

How can I keep my kidneys healthy if I have diabetes?
The best way to slow or prevent diabetes-related kidney disease is to try to reach your blood glucose and blood pressure goals. Healthy lifestyle habits and taking your medicines as prescribed can help you achieve these goals and improve your health overall.
Reach your blood glucose goals
Your health care professional will test your A1C. The A1C is a blood test that shows your average blood glucose level over the past 3 months. This is different from the blood glucose checks that you may do yourself. The higher your A1C number, the higher your blood glucose levels have been during the past 3 months.
The A1C goal for many people with diabetes is below 7 percent. Ask your health care team what your goal should be. Reaching your goal numbers will help you protect your kidneys.
To reach your A1C goal, your health care professional may ask you to check your blood glucose levels. Work with your health care team to use the results to guide decisions about food, physical activity, and medicines. Ask your health care team how often you should check your blood glucose level.

Control your blood pressure
Blood pressure is the force of your blood against the wall of your blood vessels. High blood pressure makes your heart work too hard. It can cause heart attack, stroke, and kidney disease.
Your health care team will also work with you to help you set and reach your blood pressure goal. The blood pressure goal for most people with diabetes is below 140/90 mm Hg. Ask your health care team what your goal should be.

Medicines that lower blood pressure can also help slow kidney damage. Two types of blood pressure medicines, ACE inhibitors and ARBs, play a special role in protecting your kidneys. Each has been found to slow kidney damage in people with diabetes who have high blood pressure and DKD. The names of these medicines end in –pril or –sartan. ACE inhibitors and ARBs are not safe for women who are pregnant.
Develop or maintain healthy lifestyle habits
Healthy lifestyle habits can help you reach your blood glucose and blood pressure goals. Following the steps below will also help you keep your kidneys healthy
- Stop smoking.
- Work with a dietitian to develop a diabetes meal plan and limit salt and sodium.
- Make physical activity part of your routine.
- Stay at or get to a healthy weight.
- Get enough sleep. Aim for 7 to 8 hours of sleep each night.
Learn more about these tips to manage diabetes.
Take medicines as prescribed
Medicines may be an important part of your treatment plan. Your health care professional will prescribe medicine based on your specific needs. Medicine can help you meet your blood glucose and blood pressure goals. You may need to take more than one kind of medicine to control your blood pressure.

How can I cope with the stress of managing my diabetes?
Managing diabetes isn’t always easy. Feeling stressed, sad, or angry is common when you are living with diabetes. You may know what to do to stay healthy but may have trouble sticking with your plan over time. Long-term stress can raise your blood glucose and blood pressure, but you can learn ways to lower your stress. Try deep breathing, gardening, taking a walk, doing yoga, meditating, doing a hobby, or listening to your favorite music. Learn more about healthy ways to cope with stress.
Does diabetic kidney disease get worse over time?
Kidney damage from diabetes can get worse over time. However, you can take steps to keep your kidneys healthy and help slow kidney damage to prevent or delay kidney failure. Kidney failure means that your kidneys have lost most of their ability to function—less than 15 percent of normal kidney function. However, most people with diabetes and kidney disease don’t end up with kidney failure.
If your kidneys become damaged as a result of diabetes, learn how to manage kidney disease.
References
Diabetes & Foot Problems
In this section:
- How can diabetes affect my feet?
- What can I do to keep my feet healthy?
- When should I see my health care provider about foot problems?
- Clinical Trials
Foot problems are common in people with diabetes. You might be afraid you’ll lose a toe, foot, or leg to diabetes, or know someone who has, but you can lower your chances of having diabetes-related foot problems by taking care of your feet every day. Managing your blood glucose levels, also called blood sugar, can also help keep your feet healthy.
How can diabetes affect my feet?
Over time, diabetes may cause nerve damage, also called diabetic neuropathy, that can cause tingling and pain, and can make you lose feeling in your feet. When you lose feeling in your feet, you may not feel a pebble inside your sock or a blister on your foot, which can lead to cuts and sores. Cuts and sores can become infected.
Diabetes also can lower the amount of blood flow in your feet. Not having enough blood flowing to your legs and feet can make it hard for a sore or an infection to heal. Sometimes, a bad infection never heals. The infection might lead to gangrene.
Gangrene and foot ulcers that do not get better with treatment can lead to an amputation of your toe, foot, or part of your leg. A surgeon may perform an amputation to prevent a bad infection from spreading to the rest of your body, and to save your life. Good foot care is very important to prevent serious infections and gangrene.
Although rare, nerve damage from diabetes can lead to changes in the shape of your feet, such as Charcot’s foot. Charcot’s foot may start with redness, warmth, and swelling. Later, bones in your feet and toes can shift or break, which can cause your feet to have an odd shape, such as a “rocker bottom.”

What can I do to keep my feet healthy?
Work with your health care team to make a diabetes self-care plan, which is an action plan for how you will manage your diabetes. Your plan should include foot care. A foot doctor, also called a podiatrist, and other specialists may be part of your health care team.
Include these steps in your foot care plan:
Check your feet every day
You may have foot problems, but feel no pain in your feet. Checking your feet each day will help you spot problems early before they get worse. A good way to remember is to check your feet each evening when you take off your shoes. Also check between your toes. If you have trouble bending over to see your feet, try using a mirror to see them, or ask someone else to look at your feet.
Look for problems such as
- cuts, sores, or red spots
- swelling or fluid-filled blisters
- ingrown toenails, in which the edge of your nail grows into your skin
- corns or calluses, which are spots of rough skin caused by too much rubbing or pressure on the same spot
- plantar warts, which are flesh-colored growths on the bottom of the feet
- athlete’s foot
- warm spots

If you have certain foot problems that make it more likely you will develop a sore on your foot, your doctor may recommend taking the temperature of the skin on different parts of your feet. A “hot spot” can be the first sign that a blister or an ulcer is starting.
Cover a blister, cut, or sore with a bandage. Smooth corns and calluses as explained below.
Wash your feet every day
Wash your feet with soap in warm, not hot, water. Test the water to make sure it is not too hot. You can use a thermometer (90° to 95° F is safe) or your elbow to test the warmth of the water. Do not soak your feet because your skin will get too dry.

After washing and drying your feet, put talcum powder or cornstarch between your toes. Skin between the toes tends to stay moist. Powder will keep the skin dry to help prevent an infection.
Smooth corns and calluses gently
Thick patches of skin called corns or calluses can grow on the feet. If you have corns or calluses, talk with your foot doctor about the best way to care for these foot problems. If you have nerve damage, these patches can become ulcers.

If your doctor tells you to, use a pumice stone to smooth corns and calluses after bathing or showering. A pumice stone is a type of rock used to smooth the skin. Rub gently, only in one direction, to avoid tearing the skin.
Do NOT
- cut corns and calluses
- use corn plasters, which are medicated pads
- use liquid corn and callus removers
Cutting and over-the counter corn removal products can damage your skin and cause an infection.
To keep your skin smooth and soft, rub a thin coat of lotion, cream, or petroleum jelly on the tops and bottoms of your feet. Do not put lotion or cream between your toes because moistness might cause an infection.
Trim your toenails straight across
Trim your toenails, when needed, after you wash and dry your feet. Using toenail clippers, trim your toenails straight across. Do not cut into the corners of your toenail. Gently smooth each nail with an emery board or nonsharp nail file. Trimming this way helps prevent cutting your skin and keeps the nails from growing into your skin.

Have a foot doctor trim your toenails if
- you cannot see, feel, or reach your feet
- your toenails are thick or yellowed
- your nails curve and grow into the skin
If you want to get a pedicure at a salon, you should bring your own nail tools to prevent getting an infection. You can ask your health care provider what other steps you can take at the salon to prevent infection.
Wear shoes and socks at all times
Wear shoes and socks at all times. Do not walk barefoot or in just socks – even when you are indoors. You could step on something and hurt your feet. You may not feel any pain and may not know that you hurt yourself.
Check the inside of your shoes before putting them on, to make sure the lining is smooth and free of pebbles or other objects.

Make sure you wear socks, stockings, or nylons with your shoes to keep from getting blisters and sores. Choose clean, lightly padded socks that fit well. Socks with no seams are best.
Wear shoes that fit well and protect your feet. Here are some tips for finding the right type of shoes:
- Walking shoes and athletic shoes are good for daily wear. They support your feet and allow them to “breathe.”
- Do not wear vinyl or plastic shoes, because they do not stretch or “breathe.”
- When buying shoes, make sure they feel good and have enough room for your toes. Buy shoes at the end of the day, when your feet are the largest, so that you can find the best fit.
- If you have a bunion, or hammertoes, which are toes that curl under your feet, you may need extra-wide or deep shoes.1 Do not wear shoes with pointed toes or high heels, because they put too much pressure on your toes.
- If your feet have changed shape, such as from Charcot’s foot, you may need special shoes or shoe inserts, called orthotics. You also may need inserts if you have bunions, hammertoes, or other foot problems.
When breaking in new shoes, only wear them for a few hours at first and then check your feet for areas of soreness.
Medicare Part B insurance and other health insurance programs may help pay for these special shoes or inserts. Ask your insurance plan if it covers your special shoes or inserts.
Protect your feet from hot and cold
If you have nerve damage from diabetes, you may burn your feet and not know you did. Take the following steps to protect your feet from heat:
- Wear shoes at the beach and on hot pavement.
- Put sunscreen on the tops of your feet to prevent sunburn.
- Keep your feet away from heaters and open fires.
- Do not put a hot water bottle or heating pad on your feet.

Wear socks in bed if your feet get cold. In the winter, wear lined, waterproof boots to keep your feet warm and dry.
Keep the blood flowing to your feet
Try the following tips to improve blood flow to your feet:
- Put your feet up when you are sitting.
- Wiggle your toes for a few minutes throughout the day. Move your ankles up and down and in and out to help blood flow in your feet and legs.
- Do not wear tight socks or elastic stockings. Do not try to hold up loose socks with rubber bands.
- Be more physically active. Choose activities that are easy on your feet, such as walking, dancing, yoga or stretching, swimming, or bike riding.
- Stop smoking.

Smoking can lower the amount of blood flow to your feet. If you smoke, ask for help to stop. You can get help by calling the national quitline at 1-800-QUITNOW or 1-800-784-8669. For tips on quitting, go to SmokeFree.gov.
Get a foot check at every health care visit
Ask your health care team to check your feet at each visit. Take off your shoes and socks when you’re in the exam room so they will remember to check your feet. At least once a year, get a thorough foot exam, including a check of the feeling and pulses in your feet.

Get a thorough foot exam at each health care visit if you have
- changes in the shape of your feet
- loss of feeling in your feet
- peripheral artery disease
- had foot ulcers or an amputation in the past1
Ask your health care team to show you how to care for your feet.
When should I see my health care provider about foot problems?
Call your health care provider right away if you have
- a cut, blister, or bruise on your foot that does not start to heal after a few days
- skin on your foot that becomes red, warm, or painful—signs of a possible infection
- a callus with dried blood inside of it,which often can be the first sign of a wound under the callus
- a foot infection that becomes black and smelly—signs you might have gangrene
Ask your provider to refer you to a foot doctor, or podiatrist, if needed.
Clinical Trials
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and other components of the National Institutes of Health (NIH) conduct and support research into many diseases and conditions.
What are clinical trials, and are they right for you?
Clinical trials are part of clinical research and at the heart of all medical advances. Clinical trials look at new ways to prevent, detect, or treat disease. Researchers also use clinical trials to look at other aspects of care, such as improving the quality of life for people with chronic illnesses. Find out if clinical trials are right for you.
What clinical trials are open?
Clinical trials that are currently open and are recruiting can be viewed at ClinicalTrials.gov.
References
Diabetic Eye Disease
On this page:
- What is diabetic eye disease?
- How does diabetes affect my eyes?
- How common is diabetic eye disease?
- Who is more likely to develop diabetic eye disease?
- What are the symptoms of diabetic eye disease?
- When should I see a doctor right away?
- How do doctors diagnose eye problems from diabetes?
- How do doctors treat diabetic eye disease?
- What can I do to protect my eyes?
- What if I already have some vision loss from diabetes?
What is diabetic eye disease?
Diabetic eye disease is a group of eye problems that can affect people with diabetes. These conditions include diabetic retinopathy, diabetic macular edema, cataracts, and glaucoma.
Over time, diabetes can cause damage to your eyes that can lead to poor vision or even blindness. But you can take steps to prevent diabetic eye disease, or keep it from getting worse, by taking care of your diabetes.
The best ways to manage your diabetes and keep your eyes healthy are to
- manage your blood glucose, blood pressure, and cholesterol, sometimes called the diabetes ABCs
- If you smoke, get help to quit smoking
- have a dilated eye exam once a year

Often, there are no warning signs of diabetic eye disease or vision loss when damage first develops. A full, dilated eye exam helps your doctor find and treat eye problems early—often before much vision loss can occur.
How does diabetes affect my eyes?
Diabetes affects your eyes when your blood glucose, also called blood sugar, is too high.
In the short term, you are not likely to have vision loss from high blood glucose. People sometimes have blurry vision for a few days or weeks when they’re changing their diabetes care plan or medicines. High glucose can change fluid levels or cause swelling in the tissues of your eyes that help you to focus, causing blurred vision. This type of blurry vision is temporary and goes away when your glucose level gets closer to normal.
If your blood glucose stays high over time, it can damage the tiny blood vessels in the back of your eyes. This damage can begin during prediabetes, when blood glucose is higher than normal, but not high enough for you to be diagnosed with diabetes. Damaged blood vessels may leak fluid and cause swelling. New, weak blood vessels may also begin to grow. These blood vessels can bleed into the middle part of the eye, lead to scarring, or cause dangerously high pressure inside your eye.
Most serious diabetic eye diseases begin with blood vessel problems. The four eye diseases that can threaten your sight are
Diabetic retinopathy
The retina is the inner lining at the back of each eye. The retina senses light and turns it into signals that your brain decodes, so you can see the world around you. Damaged blood vessels can harm the retina, causing a disease called diabetic retinopathy.
In early diabetic retinopathy, blood vessels can weaken, bulge, or leak into the retina. This stage is called nonproliferative diabetic retinopathy.
If the disease gets worse, some blood vessels close off, which causes new blood vessels to grow, or proliferate, on the surface of the retina. This stage is called proliferative diabetic retinopathy. These abnormal new blood vessels can lead to serious vision problems.


Diabetic macular edema
The part of your retina that you need for reading, driving, and seeing faces is called the macula. Diabetes can lead to swelling in the macula, which is called diabetic macular edema. Over time, this disease can destroy the sharp vision in this part of the eye, leading to partial vision loss or blindness. Macular edema usually develops in people who already have other signs of diabetic retinopathy.
Glaucoma
Glaucoma is a group of eye diseases that can damage the optic nerve—the bundle of nerves that connects the eye to the brain. Diabetes doubles the chances of having glaucoma, which can lead to vision loss and blindness if not treated early.
Symptoms depend on which type of glaucoma you have. Learn more about glaucoma.

Cataracts
The lenses within our eyes are clear structures that help provide sharp vision—but they tend to become cloudy as we age. People with diabetes are more likely to develop cloudy lenses, called cataracts. People with diabetes can develop cataracts at an earlier age than people without diabetes. Researchers think that high glucose levels cause deposits to build up in the lenses of your eyes.

How common is diabetic eye disease?
Diabetic retinopathy
About one in three people with diabetes who are older than age 40 already have some signs of diabetic retinopathy.1 Diabetic retinopathy is the most common cause of vision loss in people with diabetes. Each person’s outlook for the future, however, depends in large part on regular care. Finding and treating diabetic retinopathy early can reduce the risk of blindness by 95 percent.
Glaucoma and cataracts
Your chances of developing glaucoma or cataracts are about twice that of someone without diabetes.
Who is more likely to develop diabetic eye disease?
Anyone with diabetes can develop diabetic eye disease. Your risk is greater with
- high blood glucose that is not treated
- high blood pressure that is not treated
High blood cholesterol and smoking may also raise your risk for diabetic eye disease.
Some groups are affected more than others. African Americans, American Indians and Alaska Natives, Hispanics/Latinos, Pacific Islanders, and older adults are at greater risk of losing vision or going blind from diabetes.
If you have diabetes and become pregnant, you can develop eye problems very quickly during your pregnancy. If you already have some diabetic retinopathy, it can get worse during pregnancy. Changes that help your body support a growing baby may put stress on the blood vessels in your eyes. Your health care team will suggest regular eye exams during pregnancy to catch and treat problems early and protect your vision.
Diabetes that occurs only during pregnancy, called gestational diabetes, does not usually cause eye problems. Researchers aren't sure why this is the case.
Your chances of developing diabetic eye disease increase the longer you have diabetes.
What are the symptoms of diabetic eye disease?
Often there are no early symptoms of diabetic eye disease. You may have no pain and no change in your vision as damage begins to grow inside your eyes, particularly with diabetic retinopathy.
When symptoms do occur, they may include
- blurry or wavy vision
- frequently changing vision—sometimes from day to day
- dark areas or vision loss
- poor color vision
- spots or dark strings (also called floaters)
- flashes of light
Talk with your eye doctor if you have any of these symptoms.
When should I see a doctor right away?
Call a doctor right away if you notice sudden changes to your vision, including flashes of light or many more spots (floaters) than usual. You also should see a doctor right away if it looks like a curtain is pulled over your eyes. These changes in your sight can be symptoms of a detached retina, which is a medical emergency.
How do doctors diagnose eye problems from diabetes?
Having a full, dilated eye exam is the best way to check for eye problems from diabetes. Your doctor will place drops in your eyes to widen your pupils. This allows the doctor to examine a larger area at the back of each eye, using a special magnifying lens. Your vision will be blurry for a few hours after a dilated exam.
Your doctor will also
- test your vision
- measure the pressure in your eyes
Your doctor may suggest other tests, too, depending on your health history.
Most people with diabetes should see an eye care professional once a year for a complete eye exam. Your own health care team may suggest a different plan, based on your type of diabetes and the time since you were first diagnosed.
How do doctors treat diabetic eye disease?
Your doctor may recommend having eye exams more often than once a year, along with management of your diabetes. This means managing your diabetes ABCs, which include your A1c, blood pressure, and cholesterol; and quitting smoking. Ask your health care team what you can do to reach your goals.

Doctors may treat advanced eye problems with medicine, laser treatments, surgery, or a combination of these options.
Medicine
Your doctor may treat your eyes with anti-VEGF medicine, such as aflibercept, bevacizumab, or ranibizumab. These medicines block the growth of abnormal blood vessels in the eye. Anti-VEGF medicines can also stop fluid leaks, which can help treat diabetic macular edema.
The doctor will inject an anti-VEGF medicine into your eyes during office visits. You'll have several treatments during the first few months, then fewer treatments after you finish the first round of therapy. Your doctor will use medicine to numb your eyes so you don’t feel pain. The needle is about the thickness of a human hair.
Anti-VEGF treatments can stop further vision loss and may improve vision in some people.
Laser Treatment
Laser treatment, also called photocoagulation, creates tiny burns inside the eye with a beam of light. This method treats leaky blood vessels and extra fluid, called edema. Your doctor usually provides this treatment during several office visits, using medicine to numb your eyes. Laser treatment can keep eye disease from getting worse, which is important to prevent vision loss or blindness. But laser treatment is less likely to bring back vision you’ve already lost compared with anti-VEGF medicines.
There are two types of laser treatment:
- Focal/grid laser treatment works on a small area of the retina to treat diabetic macular edema.
- Scatter laser treatment, also called panretinal photocoagulation (PRP), covers a larger area of the retina. This method treats the growth of abnormal blood vessels, called proliferative diabetic retinopathy.
Vitrectomy
Vitrectomy is a surgery to remove the clear gel that fills the center of the eye, called the vitreous gel. The procedure treats problems with severe bleeding or scar tissue caused by proliferative diabetic retinopathy. Scar tissue can force the retina to peel away from the tissue beneath it, like wallpaper peeling away from a wall. A retina that comes completely loose, or detaches, can cause blindness.
During vitrectomy, a clear salt solution is gently pumped into the eye to maintain eye pressure during surgery and to replace the removed vitreous. Vitrectomy is done in a surgery center or hospital with pain medicine.
Cataract Lens Surgery
In a surgery center or hospital visit, your doctor can remove the cloudy lens in your eye, where the cataract has grown, and replace it with an artificial lens. People who have cataract surgery generally have better vision afterward. After your eye heals, you may need a new prescription for your glasses. Your vision following cataract surgery may also depend on treating any damage from diabetic retinopathy or macular edema.
What can I do to protect my eyes?
To prevent diabetic eye disease, or to keep it from getting worse, manage your diabetes ABCs: your A1c, blood pressure, and cholesterol; and quit smoking if you smoke. Read more information on how to manage diabetes.
Also, have a dilated eye exam at least once a year—or more often if recommended by your eye care professional. These actions are powerful ways to protect the health of your eyes—and can prevent blindness.
The sooner you work to manage your diabetes and other health conditions, the better. And, even if you’ve struggled in the past to manage your health, taking better care of yourself now can protect your eyes for the future. It’s never too late to begin.
What if I already have some vision loss from diabetes?
Ask your eye care professional to help you find a low vision and rehabilitation clinic. Special eye care professionals can help you manage vision loss that cannot be corrected with glasses, contact lenses, medicine, or surgery. Special devices and training may help you make the most of your remaining vision so that you can continue to be active, enjoy hobbies, visit friends and family members, and live without help from others.
References
Diabetes, Gum Disease, & Other Dental Problems
On this page:
- How can diabetes affect my mouth?
- What are the most common mouth problems from diabetes?
- How will I know if I have mouth problems from diabetes?
- What should I do if I have mouth problems from diabetes?
- How can I prepare for dental work?
- How can I keep my mouth healthy?
- Clinical Trials for Diabetes and Gum Disease
Diabetes affects many parts of your body, including your mouth. People with diabetes are more likely to have gum disease, cavities, and other problems with their teeth and gums.1 And some of these mouth problems can make your diabetes worse.
Taking good care of your teeth and gums, including getting regular cleanings and needed treatments, will help you prevent these problems or stop them from getting worse. Keeping your mouth healthy will also make it easier for you to manage your diabetes and prevent diabetes-related health problems, such as heart disease and kidney disease.1
 Good dental care can prevent mouth problems and help you manage your diabetes.
Good dental care can prevent mouth problems and help you manage your diabetes.How can diabetes affect my mouth?
Diabetes can affect your mouth by changing your saliva—the fluid that keeps your mouth wet. Saliva helps prevent tooth decay by washing away pieces of food, preventing bacteria from growing, and fighting the acids produced by bacteria. Saliva also has minerals that help protect tissues in your mouth and fight tooth decay.
Diabetes and some medicines used to treat diabetes can cause the salivary glands in your mouth to make less saliva. When less saliva flows, the risk for dental cavities, gum disease, and other mouth problems increases.
Diabetes can also increase the amount of glucose in your saliva. Diabetes occurs when your blood glucose level, also called blood sugar, is too high. High levels of glucose in your blood can also cause glucose to build up in your saliva. This glucose can feed harmful bacteria that combine with food to form a soft, sticky film called plaque, which causes cavities. If you don’t remove plaque, it can also build up on your teeth near your gum line and harden into a deposit called tartar, which can cause gum disease.
Untreated, these mouth problems can lead to tooth loss. Almost 25% of U.S. adults with diabetes ages 50 and older have severe tooth loss, compared with about 16% of those without diabetes.2
What are the most common mouth problems from diabetes?
Gum disease
Gum disease, also called periodontal gum disease, is the most common and serious mouth problem related to diabetes. Untreated, the disease advances in stages, from inflamed gums to tooth loss. High levels of blood glucose increase the risk that gum disease will progress from mild to severe.1
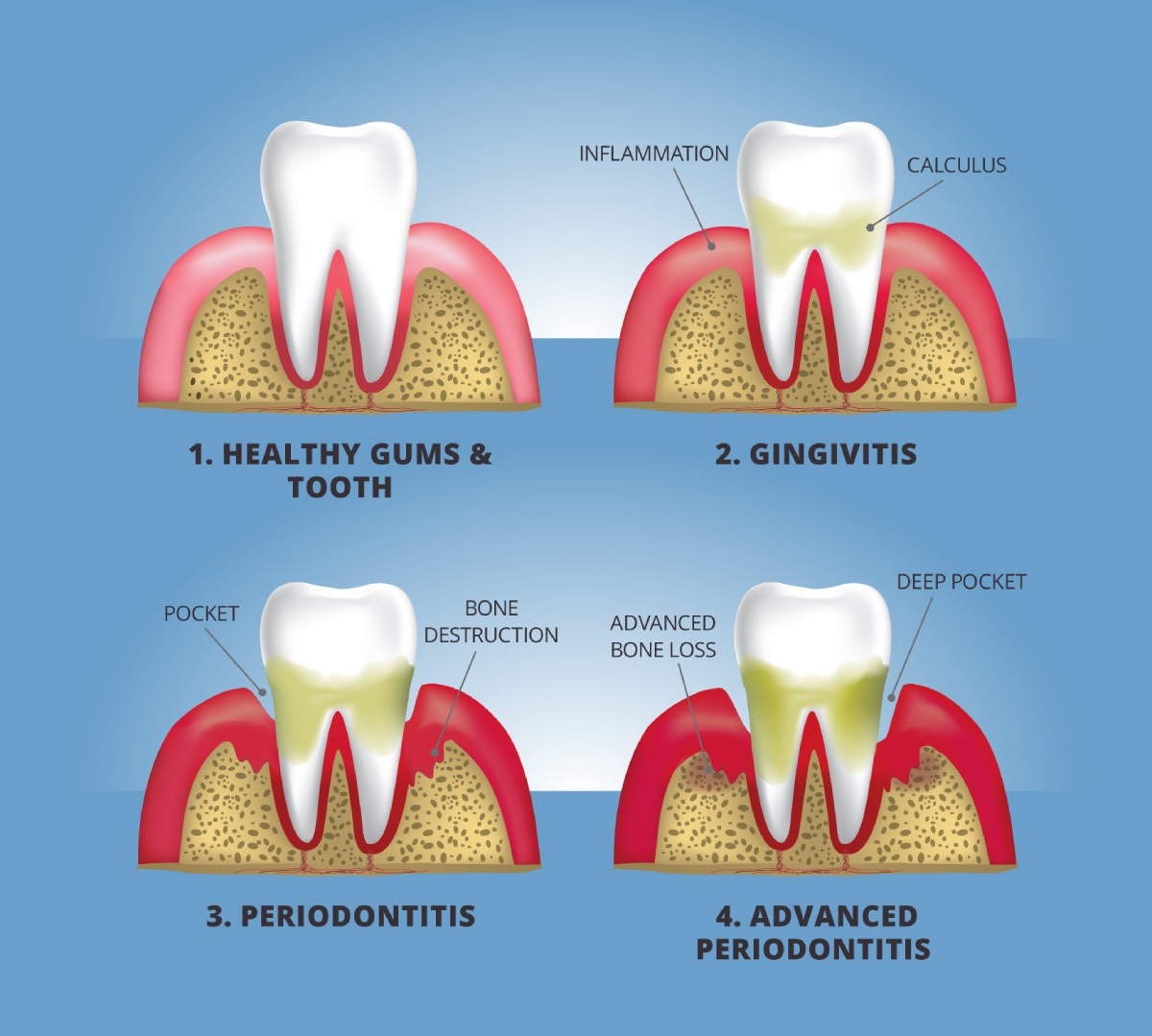 Gum disease advances in stages, from inflamed gums to tooth loss.
Gum disease advances in stages, from inflamed gums to tooth loss.
Gingivitis, or inflamed gums
The first stage of gum disease is gingivitis, a mild inflammation of the soft tissues around your teeth. Gingivitis develops when plaque and tartar build up on your teeth near your gum line, irritating and inflaming your gums. As a result, your gums may become red and swollen, and may bleed easily.
Periodontitis
Untreated, gingivitis can progress to periodontitis, an infection of the gums and bone that hold your teeth in place. Your gums may pull away from your teeth, forming pockets that slowly become infected. The bacteria in your mouth and your body’s response to the infection start to break down the bone and tissue that hold your teeth in place. If periodontitis is not treated, the teeth can become loose and may even need to be removed.
Other common mouth problems
In addition to gum disease, diabetes also increases your risk for3
- dental cavities
- dry mouth, a lack of saliva that can cause sores, ulcers, and infections
- thrush, a fungal infection that causes painful, white patches in your mouth
- burning mouth syndrome, a burning feeling inside your mouth caused by uncontrolled blood glucose levels
- changes in the way foods and beverages taste
These mouth problems, as well as tooth loss, can make it harder for you to follow a healthy meal plan that will help you manage your diabetes.
How will I know if I have mouth problems from diabetes?
Check your mouth for signs and symptoms of problems from diabetes, such as1
- gums that are
- red, swollen, or bleeding
- receding
- pulling away from your teeth
- loose teeth
- increasing spaces between your teeth
- dry mouth, an important sign of diabetes
- bad breath that doesn’t go away when you brush your teeth
 Check your mouth for signs of problems from diabetes.
Check your mouth for signs of problems from diabetes.
What should I do if I have mouth problems from diabetes?
See your dentist right away if you notice any signs or symptoms of mouth problems. Your dentist is an important ally in keeping your mouth healthy and treating mouth problems before they become serious.
If you have diabetes
- tell your dentist about your diabetes, including how long you’ve had the disease, any diabetes-related problems you may have, and any medicines you take
- keep your dentist updated on any changes to your health, including any increase in your blood glucose levels
- ask how often you should come in for regular cleanings and checkups
- follow your dentist’s advice on how to prevent and treat mouth problems from diabetes
If you feel nervous about visiting the dentist, tell your dentist and the staff about your feelings. Your dentist can adapt the treatment to your needs.
 If you notice any mouth problems, see your dentist right away.
If you notice any mouth problems, see your dentist right away.How can I prepare for dental work?
High blood glucose increases the risk for infections after mouth surgery and can also take your mouth longer to heal. Tell your doctor if you will be having oral surgery or other extensive dental work. To help you prepare for and heal after the procedure, ask your doctor
- how often you should check your blood glucose before and after the procedure
- what, if any, changes you should make to your medicines, such as changing the dose or the time you take a medicine
- how to best treat any soreness after the procedure
How can I keep my mouth healthy?
Keep your mouth healthy (PDF, 242.78 KB) by taking these steps
- Keep your blood glucose numbers within your target range. Your doctor can help set your target and explain what to do if your numbers are too high or too low.
- Consume healthy meals and beverages and follow the meal plan you and your doctor or registered dietitian have worked out.
- Visit your dentist regularly. Ask your dentist how to take care of your teeth at home, including the cleaning tools and products you should use. Your dentist can recommend a cleaning routine tailored to your needs.
Taking good care of your teeth is not always easy. Challenges can include finding a dentist nearby who can help you develop a dental routine that works for you and being able to afford dental care and related products. If you are worried about costs, consider free or low-cost dental care options, such as
- community health centers across the country that provide free or reduced-cost health services, including dental care.
- Medicaid, a state-run program that provides medical benefits to eligible individuals and families. Most states offer limited dental services for adults, while some provide comprehensive services.
Don’t let these concerns stop you from having regular checkups. Waiting too long to take care of your mouth may make things worse.
Smoking raises your risk for many diabetes problems and mouth problems. If you smoke or use other tobacco products, stop. Ask for help so you don’t have to do it alone. You can start by calling the National Quitline at 1-800-QUITNOW or 1-800-784-8669. For tips on quitting, visit Smokefree.gov.
Clinical Trials for Diabetes and Gum Disease
The NIDDK conducts and supports clinical trials in many diseases and conditions, including diabetes. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for diabetes and gum disease?
Clinical trials—and other types of clinical studies—are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help doctors and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of diabetes and gum disease, such as how certain genes may play a role in diabetes, gum disease, heart disease, and bone loss.
Find out if clinical studies are right for you.
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical studies for diabetes and gum disease are looking for participants?
You can find clinical studies on diabetes and gum disease at ClinicalTrials.gov. In addition to searching for federally funded studies, you can expand or narrow your search to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe. Always talk with your health care provider before you participate in a clinical study.
References
Diabetes, Sexual, & Bladder Problems
In this section:
- Can sexual and bladder problems be symptoms of diabetes?
- When should I see a doctor about my sexual or bladder problems?
- What makes me more likely to develop sexual or bladder problems?
- What sexual problems can men with diabetes have?
- What sexual problems can women with diabetes have?
- What bladder problems can men and women with diabetes have?
- How can I prevent and treat my sexual or bladder problems?
Sexual problems and bladder problems are common as people age, but diabetes can make these problems worse. You or your partner may have trouble having or enjoying sex. Or, you may leak urine or have trouble emptying your bladder normally.
Blood vessels and nerves can be damaged by the effects of high blood glucose, also called blood sugar. This damage can lead to sexual and bladder problems. Keeping your blood glucose levels in your target range is an important way to prevent damage to your blood vessels and nerves.
Work with your health care team to help prevent or treat sexual and bladder problems. These problems may be signs that you need to manage your diabetes in a different way. Remember, a healthy sex life and a healthy bladder can improve your quality of life, so take action now if you have concerns.

Can sexual and bladder problems be symptoms of diabetes?
Yes. Changes in sexual function or bladder habits may be a sign that you have diabetes. Nerve damage caused by diabetes, also called diabetic neuropathy, can damage parts of your body—like your genitals or urinary tract. For example, men with diabetes may develop erectile dysfunction (ED) 10 to 15 years earlier than men without diabetes.1
Talk with a health care professional if you have any symptoms of diabetes, including sexual and bladder problems.
When should I see a doctor about my sexual or bladder problems?
See a health care professional for problems with sex or your bladder. These problems could be a sign that you need to manage your diabetes differently. You may find it embarrassing and difficult to talk about these things. However, remember that health care professionals are trained to speak with people about every kind of health problem. Everyone deserves to have healthy relationships and enjoy the activities they love.
What makes me more likely to develop sexual or bladder problems
You’re more likely to develop sexual or bladder problems if you have diabetes and
- have high blood glucose that is not well controlled, also called high blood sugar
- have nerve damage, also called neuropathy
- have high blood pressure that is not treated
- have high cholesterol that is not treated
- are overweight or have obesity
- are not physically active
- are taking certain medicines
- drink too many alcoholic drinks
- smoke
Research also suggests that certain genes may make people more likely to develop diabetic neuropathy.2
What sexual problems can men with diabetes have?
Changes in your blood vessels, nerves, hormones, and emotional health during diabetes may make it more difficult for you to have satisfactory sex. Diabetes and its related challenges also may make it harder for you to have a child.
Erectile dysfunction
You have ED if you’re unable to get or keep an erection firm enough for satisfactory sexual intercourse. More than half of men with diabetes will get ED. Men who have diabetes are more than 3 times more likely to develop ED than men who do not have diabetes.1 Good diabetes management may help prevent and treat ED caused by nerve damage and circulation problems. A doctor can help treat ED with medicine or a change in your diabetes care plan.

Retrograde ejaculation
Rarely, diabetes can cause retrograde ejaculation, which is when part or all of your semen goes into your bladder instead of out of your penis during ejaculation. During retrograde ejaculation, semen enters your bladder, mixes with urine, and is safely urinated out. A urine sample after ejaculation can show if you have retrograde ejaculation. Some men with retrograde ejaculation may not ejaculate at all.
Penile curvature
Men with diabetes are more likely to have Peyronie’s disease, also called penile curvature, than men who don’t have diabetes.3 Men with Peyronie’s disease have scar tissue, called a plaque, in the penis, making it curve when erect. Curves in the penis can make sexual intercourse painful or difficult. Some men with Peyronie’s disease may have ED.
Low testosterone
Men’s testosterone levels naturally lower with age. However, lower-than-normal testosterone levels may be the cause of some men’s ED, or can explain why some men often feel tired, depressed, or have a low sex drive. Men with diabetes, especially those who are older and overweight, are more likely to have low testosterone, or “low T.”
If your doctor thinks you might have low T, you will probably be asked to give a blood sample, and a health care professional will give you a physical exam. Your doctor may suggest treating your low testosterone with a prescription gel, injection, or patch.
Several studies show that, along with good diabetes management, testosterone therapy can lessen a man’s sexual problems.4 However, testosterone therapy may have serious risks and may not be safe for all men. Talk with your doctor about testosterone therapy’s side effects and whether it’s right for you.
Fertility problems
Some studies show that men with diabetes can have problems with their sperm that make it harder to conceive. Your sperm could be slow or not move well, or your sperm may not be able to fertilize a woman’s egg well.5 Working closely with your partner and a health care professional trained in fertility issues may help.
If you and your partner want to conceive a child, your doctor may treat retrograde ejaculation caused by diabetes with medicine or by changing your diabetes care plan. Or, talk with a urologist who is a fertility expert. He or she may be able to collect your sperm from your urine and then use it for artificial insemination.
What sexual problems can women with diabetes have?
Low sexual desire and response, vaginal dryness, and painful sex can be caused by nerve damage, reduced blood flow to the genitals, and hormonal changes. Other conditions can cause these problems, too, including menopause. If you notice a change in your sex life, talk with your health care team. A physical exam, which will include a pelvic exam, and blood and urine tests may help your doctor find the cause of your problems.
Low sexual desire and response
Low sexual desire and sexual response can include
- being unable to become or stay aroused
- not having enough vaginal lubrication
- having little to no feeling in your genitals
- being unable to have an orgasm or rarely having one
With diabetes, your body and mind will likely go through many changes. For example, both high and low blood glucose levels can affect how and if you become aroused. Or, you may find yourself more tired than usual or depressed and anxious, making you less interested in sex.
Your health care team can help you make changes to your diabetes care plan so that you‘re back on track. Women who keep blood glucose levels in their target range are less likely to have nerve damage, which can lead to low sexual desire and response.
Painful sex
Some women with diabetes say they have uncomfortable or painful sexual intercourse. The nerves that tell your vagina to lubricate during stimulation can become damaged by diabetes. A prescription or over-the-counter vaginal lubricant may help if you have vaginal dryness. Managing your blood glucose well over many weeks, months, and years can help prevent nerve damage.
Yeast and bladder infections
Women with diabetes are more likely to have yeast infections, because yeast organisms can grow more easily when your blood glucose levels are higher. Yeast infections can be uncomfortable or painful and prevent you from enjoying activities, including having sex.
Although some yeast infections can be treated at home, talk with a health care professional first about your symptoms. Some symptoms of yeast infections are similar to other types of infections, including sexually transmitted diseases.
Pregnancy concerns and fertility problems
If you have diabetes and plan to become pregnant, it’s important to get your blood glucose levels close to your target range before you get pregnant. High blood glucose can harm your baby during the first weeks of pregnancy, even before you know you’re pregnant.
If you have diabetes and are already pregnant, see your doctor as soon as possible to make a plan to manage your diabetes. Working with your health care team and following your diabetes management plan can help you have a healthy pregnancy and a healthy baby.
Health problems such as obesity and polycystic ovary syndrome (PCOS) that are linked to diabetes can make it harder to conceive a child. Talk with a health care professional, such as a gynecologist or a fertility specialist, if you’re having problems conceiving a child.

What bladder problems can men and women with diabetes have?
Diabetes can cause nerve damage to your urinary tract, causing bladder problems. Overweight and obesity also can increase bladder problems, such as urinary incontinence (UI). Managing diabetes is an important part of preventing problems that can lead to excess urination.
Your health care team may be able to help you manage your blood glucose levels and help you lose weight, if needed. Doctors use blood and urine tests to diagnose bladder problems or conditions with similar symptoms. Doctors also may use urodynamic testing to see what kind of bladder problem you have.
Frequent and urgent urination
Some people with diabetes who regularly have high blood glucose levels may have to urinate too often, also called urinary frequency. Even men and women with diabetes who manage their blood glucose levels within their target range sometimes feel the sudden urge to urinate, called urgency incontinence. This can happen at night, also. Medicines may help reduce the symptoms of bladder control problems.
Trouble “going”
You may find that diabetes causes you to no longer feel when your bladder is full. Many people with diabetes report that they have trouble “going.” Over time, having a too-full bladder can cause damage to your bladder muscles that push urine out. When these muscles don’t work correctly, urine may stay in your bladder too long, also called urinary retention. Urinary retention can cause bladder infections, urine leaks, and the feeling that you always have to go.
Leaking urine
People with diabetes are more likely to have other types of UI, such as stress incontinence. Nerve damage, obesity, and bladder infections, which are linked with diabetes, are often related to bladder control problems. Leaking urine can cause you to avoid activities you once enjoyed, including sex.
If you’re overweight, losing weight can help you have fewer leaks. Avoiding weight gain may prevent UI. Studies suggest that, as your body mass index (BMI) increases, you’re more likely to leak.6 If you’re overweight or have obesity, talk with your doctor about how to lose weight.
Work with your health care team to help manage and prevent urine leaks. Bladder control problems are often treatable and are very common, even in people who don’t have diabetes. You don’t have to accept rushing to the bathroom all the time to avoid leaks.
Bladder infections
People with diabetes are more likely to have urinary tract infections, also called bladder infections, or cystitis. See a doctor right away if you have frequent, urgent urination that may be painful. Bladder infections can develop into kidney infections and can make bladder symptoms, such as leaks and urine retention, worse. Also, bladder infections can get in the way of your everyday life, including intimacy. Managing your blood glucose levels can help prevent bladder infections.

How can I prevent and treat my sexual or bladder problems?
Managing your diabetes can help prevent nerve damage and other diabetes problems that can lead to sexual and bladder problems. With your health care team, you can help prevent and treat your sexual or bladder control problems by
- keeping your blood glucose, blood pressure, and cholesterol levels close to your target numbers
- being physically active
- keeping a healthy weight
- quitting smoking if you smoke
- getting help for any emotional or psychological problems
Sex is a physical activity, so be sure to check your blood glucose level before and after sex, especially if you take insulin. Both high blood glucose levels and low blood glucose levels can cause problems during sex.
Counseling may also be helpful when you notice changes in your sexual function or desire. These types of changes are very common as people age or adjust to health problems.
If you have a partner, he or she also may be an important member of your health care team. You may find it helpful to share your concerns and have that person join you at the doctor’s office or at counseling. Your friends and family may also be able to support you if you’re having bladder problems.
References
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.

