Pancreatitis
Return to Overview PageDefinition & Facts
In this section:
- What is pancreatitis?
- How common is pancreatitis?
- Who is more likely to get pancreatitis?
- What are the complications of pancreatitis?
What is pancreatitis?
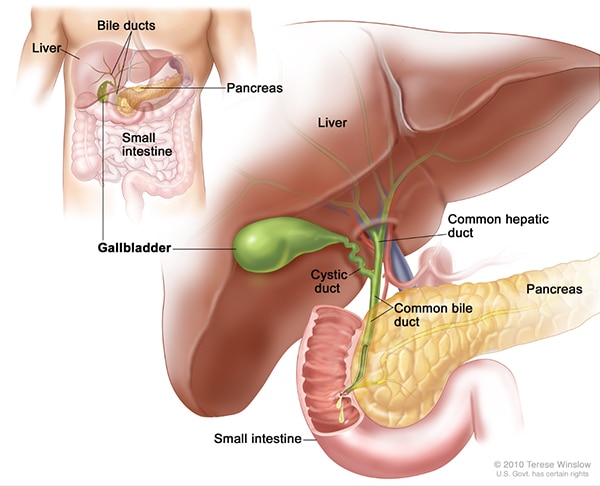
Pancreatitis is inflammation of the pancreas. The pancreas is a large gland behind the stomach, close to the first part of the small intestine, called the duodenum. The pancreas has two main functions—to make insulin and to make digestive juices, or enzymes, to help you digest food. These enzymes digest food in the intestine. Pancreatitis occurs when the enzymes damage the pancreas, which causes inflammation. Pancreatitis can be acute or chronic. Either form is serious and can lead to complications.
Acute pancreatitis
Acute pancreatitis occurs suddenly and is a short-term condition. Most people with acute pancreatitis get better, and it goes away in several days with treatment. Some people can have a more severe form of acute pancreatitis, which requires a lengthy hospital stay.
Chronic pancreatitis
Chronic pancreatitis is a long-lasting condition. The pancreas does not heal or improve. Instead, it gets worse over time, which can lead to lasting damage to your pancreas.
How common is pancreatitis?
Acute pancreatitis has becoming more common, for reasons that are not clear. Each year, about 275,000 hospital stays for acute pancreatitis occur in the United States.1 Although pancreatitis is rare in children, the number of children with acute pancreatitis has grown.
Chronic pancreatitis is less common, with about 86,000 hospital stays per year.2
Who is more likely to get pancreatitis?
Certain groups of people are more likely to get acute or chronic pancreatitis than others:
- Men are more likely to get pancreatitis than women.1
- African Americans have a higher risk of getting pancreatitis.3
- People with a family history of pancreatitis have a higher risk.
- People with a personal or family history of gallstones also have a higher risk.
People with certain health conditions
You are more likely to get pancreatitis if you have one of the following health conditions:
- diabetes
- gallstones
- high triglycerides
- genetic disorders of the pancreas
- certain autoimmune conditions
- cystic fibrosis
People with other health concerns
You are also more likely to get pancreatitis if you
- have obesity
- are a heavy alcohol user
- are a smoker
What are the complications of pancreatitis?
Both acute and chronic pancreatitis can lead to complications that include
- narrowing or blockage in a bile or pancreatic duct
- leakage from the pancreatic duct
- pancreatic pseudocysts
- damage to your pancreas
- heart, lung, or kidney failure
- death
Acute pancreatitis
Repeat episodes of acute pancreatitis may lead to chronic pancreatitis. Other complications of acute pancreatitis include
- dehydration
- bleeding
- infection
Chronic pancreatitis
Complications of chronic pancreatitis include
- chronic pain in your abdomen
- maldigestion, when you can’t digest food properly
- malnutrition and malabsorption
- problems with how well your pancreas works
- scars in your pancreas
- diabetes
- pancreatic cancer, which is more likely in people with both diabetes and pancreatitis
- osteopenia, osteoporosis, and bone fractures
References
Symptoms & Causes
What are the symptoms of pancreatitis?
The main symptom of acute and chronic pancreatitis is
- pain in your upper abdomen that may spread to your back
People with acute or chronic pancreatitis may feel the pain in different ways.
Acute pancreatitis
Acute pancreatitis usually starts with pain that
- begins slowly or suddenly in your upper abdomen
- sometimes spreads to your back
- can be mild or severe
- may last for several days
Other symptoms may include
People with acute pancreatitis usually look and feel seriously ill and need to see a doctor right away.

Chronic pancreatitis
Most people with chronic pancreatitis
- feel pain in the upper abdomen, although some people have no pain at all.
The pain may
- spread to your back
- become constant and severe
- become worse after eating
- go away as your condition gets worse
People with chronic pancreatitis may not have symptoms until they have complications.
Other symptoms may include
Seek care right away for pancreatitis
Seek care right away for the following symptoms of severe pancreatitis:
- pain or tenderness in the abdomen that is severe or becomes worse
- nausea and vomiting
- fever or chills
- fast heartbeat
- shortness of breath
- yellowish color of the skin or whites of the eyes, called jaundice
These symptoms may be a sign of
- serious infection
- inflammation
- blockage of the pancreas, gallbladder, or a bile and pancreatic duct
Left untreated, these problems can be fatal.
What causes pancreatitis?
The most common causes of both acute and chronic pancreatitis are
- gallstones
- heavy alcohol use
- genetic disorders of your pancreas
- some medicines
Other causes include
- infections, such as viruses or parasites
- injury to your abdomen
- pancreatic cancer
- having a procedure called endoscopic retrograde cholangiopancreatography (ERCP) to treat another condition
- pancreas divisum
Acute pancreatitis
The most common cause of acute pancreatitis is having gallstones.
Gallstones cause inflammation of your pancreas as stones pass through and get stuck in a bile or pancreatic duct. This condition is called gallstone pancreatitis.
Chronic pancreatitis
The most common causes of chronic pancreatitis are
- heavy alcohol use
- genetic disorders of your pancreas
Other causes include
- blockage in your pancreatic duct
- high levels of blood fats, called lipids
- high level of calcium in your blood
In many cases, doctors can’t find the cause of pancreatitis. This is called idiopathic pancreatitis.
Diagnosis
How do doctors diagnose pancreatitis?
To diagnose pancreatitis and find its causes, doctors use
- your medical history
- a physical exam
- lab and imaging tests
A health care professional will ask
- about your symptoms
- if you have a history of health conditions or concerns that make you more likely to get pancreatitis—including medicines you are taking
- if you have a personal or family medical history of pancreatitis or gallstones
During a physical exam, the health care professional will
- examine your body
- check your abdomen for pain, swelling, or tenderness

What tests do health care professionals use to diagnose pancreatitis?
Health care professionals may use lab or imaging tests to diagnose pancreatitis and find its causes. Diagnosing chronic pancreatitis can be hard in the early stages. Your doctor will also test for other conditions that have similar symptoms, such as peptic ulcers or pancreatic cancer.
Lab tests
Lab tests to help diagnose pancreatitis include the following:
Blood tests. A health care professional may take a blood sample from you and send the sample to a lab to test for
- high amylase and lipase levels—digestive enzymes made in your pancreas
- high blood glucose, also called blood sugar
- high levels of blood fats, called lipids
- signs of infection or inflammation of the bile ducts, pancreas, gallbladder, or liver
- pancreatic cancer
Stool tests. Your doctor may test a stool sample to find out if a person has fat malabsorption.
Imaging tests
Health care professionals also use imaging tests to diagnose pancreatitis. A technician performs most tests in an outpatient center, a hospital, or a doctor’s office. You don’t need anesthesia, a medicine to keep you calm, for most of these tests.
Ultrasound. Ultrasound uses a device called a transducer, which bounces safe, painless sound waves off your organs to create a picture of their structure. Ultrasound can find gallstones.
Computed tomography (CT) scan. CT scans create pictures of your pancreas, gallbladder, and bile ducts. CT scans can show pancreatitis or pancreatic cancer.
Magnetic resonance cholangiopancreatography (MRCP). MRCP uses a magnetic resonance imaging (MRI) machine, which creates pictures of your organs and soft tissues without x-rays. Your doctor or a specialist may use MRCP to look at your pancreas, gallbladder, and bile ducts for causes of pancreatitis.

Endoscopic ultrasound (EUS). Your doctor inserts an endoscope—a thin, flexible tube—down your throat, through your stomach, and into your small intestine. The doctor turns on an ultrasound attachment to create pictures of your pancreas and bile ducts. Your doctor may send you to a gastroenterologist to perform this test.
Pancreatic Function Test (PFT). Your doctor may use this test to measure how your pancreas responds to secretin, a hormone made by the small intestine. This test is done only at some centers in the United States.
Treatment
How do health care professionals treat pancreatitis?
Treatment for acute or chronic pancreatitis may include
- a hospital stay to treat dehydration with intravenous (IV) fluids and, if you can swallow them, fluids by mouth
- pain medicine, and antibiotics by mouth or through an IV if you have an infection in your pancreas
- a low-fat diet, or nutrition by feeding tube or IV if you can’t eat
Your doctor may send you to a gastroenterologist or surgeon for one of the following treatments, depending on the type of pancreatitis that you have.
Acute pancreatitis
Mild acute pancreatitis usually goes away in a few days with rest and treatment. If your pancreatitis is more severe, your treatment may also include:
Surgery. Your doctor may recommend surgery to remove the gallbladder, called cholecystectomy, if gallstones cause your pancreatitis. Having surgery within a few days after you are admitted to the hospital lowers the chance of complications. If you have severe pancreatitis, your doctor may advise delaying surgery to first treat complications.
Procedures. Your doctor or specialist will drain fluid in your abdomen if you have an abscess or infected pseudocyst, or a large pseudocyst causing pain or bleeding. Your doctor may remove damaged tissue from your pancreas.
Endoscopic Cholangiopancreatography (ERCP). Doctors use ERCP to treat both acute and chronic pancreatitis. ERCP combines upper gastrointestinal endoscopy and x-rays to treat narrowing or blockage of a bile or pancreatic duct. Your gastroenterologist may use ERCP to remove gallstones blocking the bile or pancreatic ducts.
Chronic pancreatitis
Treatment for chronic pancreatitis may help relieve pain, improve how well the pancreas works, and manage complications.
Your doctor may prescribe or provide the following:
Medicines and vitamins. Your doctor may give you enzyme pills to help with digestion, or vitamins A, D, E, and K if you have malabsorption. He or she may also give you vitamin B-12 shots if you need them.
Treatment for diabetes. Chronic pancreatitis may cause diabetes. If you get diabetes, your doctor and health care team will work with you to create an eating plan and a routine of medicine, blood glucose monitoring, and regular checkups.
Surgery. Your doctor may recommend surgery to relieve pressure or blockage in your pancreatic duct, or to remove a damaged or infected part of your pancreas. Surgery is done in a hospital, where you may have to stay a few days.
In patients who do not get better with other treatments, surgeons may perform surgery to remove your whole pancreas, followed by islet auto-transplantation. Islets are groups of cells in your pancreas that make hormones, including insulin. After removing your pancreas, doctors will take islets from your pancreas and transplant them into your liver. The islets will begin to make hormones and release them into your bloodstream.
Procedures. Your doctor may suggest a nerve block, which is a shot of numbing medicine through your skin and directly into nerves that carry the pain message from your pancreas. If you have stones blocking your pancreatic duct, your doctor may use a procedure to break up and remove the stones.

How can I help manage my pancreatitis?
Stop drinking alcohol
Health care professionals strongly advise people with pancreatitis to stop drinking alcohol, even if your pancreatitis is mild or in the early stages. Continuing to drink alcohol when you have acute pancreatitis can lead to
- more episodes of acute pancreatitis
- chronic pancreatitis
When people with chronic pancreatitis caused by alcohol use continue to drink alcohol, the condition is more likely to lead to severe complications and even death.
Talk with your health care professional if you need help to stop drinking alcohol.
Stop smoking
Health care professionals strongly advise people with pancreatitis to stop smoking, even if your pancreatitis is mild or in the early stages. Smoking with acute pancreatitis, especially if it’s caused by alcohol use, greatly raises the chances that your pancreatitis will become chronic. Smoking with pancreatitis also may raise your risk of pancreatic cancer.
Talk with your health care professional if you need help to stop smoking.
How can I help prevent pancreatitis?
You can’t prevent pancreatitis, but you can take steps to help you stay healthy.
Maintain a healthy weight or lose weight safely
Maintaining a healthy lifestyle and a healthy weight—or losing weight if needed—can help to
- make your pancreas work better
- lower your chance of getting gallstones, a leading cause of pancreatitis
- prevent obesity—a risk factor for pancreatitis
- prevent diabetes—a risk factor for pancreatitis

Avoid alcohol use
Alcohol use can cause acute and chronic pancreatitis. Talk with your health care professional if you need help to stop drinking alcohol.
Avoid smoking
Smoking is a common risk factor for pancreatitis—and the chances of getting pancreatitis are even higher in people who smoke and drink alcohol. Talk with your health care professional if you need help to stop smoking.
Eating, Diet, & Nutrition
Can what I eat help or prevent pancreatitis?
During pancreatitis treatment, your doctor may tell you not to eat or drink for a while. Instead, your doctor may use a feeding tube to give you nutrition. Once you may start eating again, he or she will prescribe a healthy, low-fat eating plan that includes small, frequent meals.

If you have pancreatitis, drink plenty of fluids and limit caffeine. Health care professionals strongly advise people with pancreatitis not to drink any alcohol, even if your pancreatitis is mild.
Having an eating plan high in fat and calories can lead to high levels of fat in your blood, which raises your risk of pancreatitis. You can lower your chances of getting pancreatitis by sticking with a low-fat, healthy eating plan.
Clinical Trials
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and other components of the National Institutes of Health (NIH) conduct and support research into many diseases and conditions.
What are clinical trials and are they right for you?
Clinical trials are part of clinical research and at the heart of all medical advances. Clinical trials look at new ways to prevent, detect, or treat disease. Researchers also use clinical trials to look at other aspects of care, such as improving the quality of life for people with chronic illnesses. Find out if clinical trials are right for you.
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical trials are open?
Clinical trials that are currently open and are recruiting can be viewed at ClinicalTrials.gov.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
The NIDDK would like to thank:
Christopher E. Forsmark, M.D., University of Florida College of Medicine

