Nonalcoholic Fatty Liver Disease & NASH
Return to Overview PageDefinition & Facts
In this section:
- What is NAFLD?
- How common is NAFLD?
- Who is more likely to develop NAFLD?
- What are the complications of NAFLD?
What is NAFLD?
Nonalcoholic fatty liver disease, or NAFLD (also referred to as metabolic dysfunction-associated steatotic liver disease, or MASLD), is a condition in which excess fat builds up in your liver. This buildup of fat is not caused by heavy alcohol use. When heavy alcohol use causes fat to build up in the liver, this condition is called alcohol-associated liver disease.
Two types of NAFLD are nonalcoholic fatty liver, or NAFL (also referred to as metabolic dysfunction-associated steatotic liver, or MASL), and nonalcoholic steatohepatitis, or NASH (also referred to as metabolic dysfunction-associated steatohepatitis, or MASH). People typically develop one type of NAFLD or the other, although sometimes people with one form are later diagnosed with the other form of NAFLD.
NAFL
NAFL is a form of NAFLD in which you have fat in your liver but little or no inflammation or liver damage. NAFL typically does not progress to cause liver damage or complications. However, NAFL can cause pain from enlargement of the liver.
NASH
NASH is the form of NAFLD in which you have inflammation of the liver and liver damage, in addition to fat in your liver. The inflammation and liver damage of NASH can cause fibrosis, or scarring, of the liver. NASH may lead to cirrhosis, in which the liver is scarred and permanently damaged. Cirrhosis can lead to liver cancer.
Experts are not sure why some people with NAFLD have NASH while others have NAFL.
How common is NAFLD?
NAFLD is one of the most common causes of liver disease in the United States. The majority of people with NAFLD have NAFL. Only a small number of people with NAFLD have NASH. Experts estimate about 24% of U.S. adults have NAFLD and about 1.5% to 6.5% of U.S. adults have NASH.1
Who is more likely to develop NAFLD?
NAFLD is more common in people who have certain diseases and conditions, including obesity, and conditions that may be related to obesity, such as type 2 diabetes. Studies suggest that one-third to two-thirds of people with type 2 diabetes have NAFLD.1 Research also suggests that NAFLD is present in up to 75% of people who are overweight and in more than 90% of people who have severe obesity.2, 3
 NAFLD is more common in people who have obesity.
NAFLD is more common in people who have obesity.NAFLD can affect people of any age, including children. Research suggests that close to 10% of U.S. children ages 2 to 19 have NAFLD.4 However, people are more likely to develop NAFLD as they age.
While NAFLD occurs in people of all races and ethnicities, it is most common among Hispanic individuals, followed by non-Hispanic whites and Asian Americans, including those of East Asian and South Asian descent.5,6 NAFLD is less common among non-Hispanic Blacks.5 On average, Asian Americans with NAFLD have a lower BMI than non-Hispanic whites with NAFLD.6 Experts think that genes may help explain some of the racial and ethnic differences in NAFLD.
What are the complications of NAFLD?
People with NAFLD may develop liver complications or other health problems.
Liver complications
People with NAFL typically don’t develop liver complications, although they have a higher risk for other health problems.1
People with NASH can develop liver complications, such as cirrhosis and liver cancer. If cirrhosis leads to liver failure, you may need a liver transplant. People with NASH have an increased chance of dying from liver-related causes.5
Other health problems
People with NAFLD have a higher risk for certain health problems, including
- cardiovascular disease, which is the most common cause of death in people who have NAFLD5
- type 2 diabetes
- metabolic syndrome
- conditions that may be part of metabolic syndrome, such as high blood pressure and abnormal levels of fats—cholesterol and triglycerides—in the blood.
References
Symptoms & Causes
What are the symptoms of NAFLD?
Usually, nonalcoholic fatty liver disease, or NAFLD (also referred to as metabolic dysfunction-associated steatotic liver disease, or MASLD), is a silent disease with few or no symptoms. You may not have symptoms even if you develop cirrhosis due to nonalcoholic steatohepatitis, or NASH (also referred to as metabolic dysfunction-associated steatohepatitis, or MASH).
If you do have symptoms, you may feel tired or have discomfort in the upper right side of your abdomen.
What causes NAFLD?
Experts are still studying the causes of NAFLD. Research suggests that certain health conditions or diseases, your genes, and diet and the digestive system may make you more likely to develop NAFLD.
Health conditions and diseases
You are more likely to develop NAFLD if you have the following health conditions or diseases
- overweight or obesity
- insulin resistance or type 2 diabetes
- abnormal levels of fats in your blood, which may include
- high levels of triglycerides
- abnormal levels of cholesterol—high total cholesterol, high LDL cholesterol, or low HDL cholesterol
- metabolic syndrome or one or more traits of metabolic syndrome. Metabolic syndrome is a group of traits and medical conditions linked to overweight and obesity. Doctors define metabolic syndrome as the presence of any three of the following
- large waist size
- high levels of triglycerides in your blood
- low levels of HDL cholesterol in your blood
- high blood pressure
- higher than normal blood glucose levels or a diagnosis of type 2 diabetes
Having more of these health conditions increases your chances of developing NASH. Losing weight may cause NASH to switch to nonalcoholic fatty liver, or NAFL (also referred to as metabolic dysfunction-associated steatotic liver, or MASL), and regaining weight may cause NAFL to switch to NASH.
Genes
Researchers have found that certain genes may make you more likely to develop NAFLD. These genes may help explain why NAFLD is more common in certain racial and ethnic groups. Experts are still studying the genes that may play a role in NAFLD.
Diet and the digestive system
Researchers are studying whether diets high in fructose—a sugar that is part of table sugar and is also commonly added to sweeten drinks and foods—may increase the risk of NAFLD.
Scientists have also examined the relationship between NAFLD and the microbiome—the bacteria in your digestive tract that help with digestion. Studies have found differences between the microbiomes of people who have NAFLD and those who don’t. Experts are still studying how the microbiome may affect NAFLD.
Is NAFLD the only cause of fatty liver?
Fatty liver may have causes other than NAFLD. If medical tests suggest you have a buildup of fat in your liver, your doctor may ask questions or order tests for other causes.
Alcohol-associated liver disease
Fat may build up in the liver due to alcohol-associated liver disease—damage to the liver and its function due to excessive alcohol consumption. If you have a history of heavy alcohol use and fat in your liver, your doctor may determine you have alcohol-associated liver disease instead of NAFLD.
If you have risks for NAFLD and also drink excessively, you could have both NAFLD and alcohol-associated liver disease at the same time. No tests can easily tell how much each plays a role.
Other causes
Other causes of excess fat in the liver include
- disorders, called lipodystrophies, that cause your body to use or store fat improperly
- rapid weight loss or malnutrition
- some medicines, including corticosteroids, HIV treatment, estrogens, certain medicines used to treat cancer, and others
- exposure to some toxins
- rare genetic diseases, such as Wilson disease and hypobetalipoproteinemia
Diagnosis
How do doctors diagnose NAFLD?
Doctors use your medical history, a physical exam, and tests to diagnose nonalcoholic fatty liver disease, or NAFLD (also referred to as metabolic dysfunction-associated steatotic liver disease, or MASLD).
Medical history
Your doctor will ask if you have a history of health conditions or diseases that make you more likely to develop NAFLD, such as
- overweight or obesity
- insulin resistance or type 2 diabetes
- high levels of triglycerides or abnormal levels of cholesterol in your blood
- metabolic syndrome
Your doctor will ask about diet and lifestyle factors that may make you more likely to develop NAFLD, such as a lack of physical activity, eating a diet high in sugar, or drinking sugary beverages.
Your doctor will also ask about other causes of liver disease or fat in your liver. Your doctor will ask about your alcohol intake to find out whether fat in your liver is a sign of alcohol-associated liver disease or NAFLD.
 Your doctor will ask if you have a history of health conditions that make you more likely to develop NAFLD.
Your doctor will ask if you have a history of health conditions that make you more likely to develop NAFLD.Physical exam
During a physical exam, a doctor usually examines your body and checks your weight and height to calculate your body mass index.
Your doctor will also look for signs of nonalcoholic fatty liver, or NAFL (also referred to as metabolic dysfunction-associated steatotic liver, or MASL), or nonalcoholic steatohepatitis, or NASH (also referred to as metabolic dysfunction-associated steatohepatitis, or MASH), such as
- an enlarged liver
- signs of insulin resistance, such as darkened skin patches over your knuckles, elbows, and knees
- signs of cirrhosis, such as an enlarged spleen, ascites, and muscle loss
What tests do doctors use to diagnose NAFLD?
Doctors use blood tests, imaging tests, and sometimes liver biopsy to diagnose NAFLD and to tell the difference between NAFL and NASH.
Blood tests
A health care professional may take a blood sample from you and send the sample to a lab. Your doctor may suspect you have NAFLD if your blood test shows increased levels of the liver enzymes alanine aminotransferase (ALT) and aspartate aminotransferase (AST).
Your doctor may use the results of routine blood tests to calculate special scores, such as the FIB-4 or APRI. These scores can help doctors identify or rule out advanced liver fibrosis, or scarring.
Your doctor may perform additional blood tests to find out if you have other health conditions that may increase your liver enzyme levels.
Imaging tests
Routine imaging tests can show fat in your liver. These tests can’t show inflammation or fibrosis, so your doctor can’t use these tests to find out whether you have NAFL or NASH. If you have cirrhosis, routine imaging tests may show nodules, or lumps, in your liver.
Your doctor may use the following imaging tests to help diagnose NAFLD
- ultrasound, which uses a device called a transducer that bounces safe, painless sound waves off your organs to create an image of their structure
- computed tomography (CT) scan, which uses a combination of x-rays and computer technology to create images of your liver
- magnetic resonance imaging (MRI), which uses radio waves and magnets to produce detailed images of organs and soft tissues without using x-rays
Elastography is a newer type of imaging test that can help determine if you have advanced liver fibrosis. In some cases, doctors may order elastography tests to measure the stiffness of your liver. Increased liver stiffness may be a sign of fibrosis. Commonly used types of elastography are
- vibration-controlled transient elastography, a special type of ultrasound
- sheer wave elastography, another type of ultrasound to detect increased liver stiffness
- magnetic resonance elastography, a special type of MRI to measure liver stiffness
Liver biopsy
Liver biopsy is the only test that can prove a diagnosis of NASH and show clearly how severe the disease is. Liver biopsy can show fibrosis at earlier stages than elastography can. However, doctors don’t recommend liver biopsy for everyone with suspected NAFLD. Your doctor may recommend a liver biopsy if you are more likely to have NASH with advanced fibrosis or if your other tests show signs of advanced liver disease or cirrhosis. In some cases, doctors may recommend a liver biopsy to rule out other liver diseases.
During a liver biopsy, a doctor will take small pieces of tissue from your liver. A pathologist will examine the tissue under a microscope to look for signs of damage or disease.
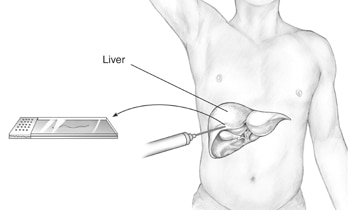 During a liver biopsy, a doctor will take a piece of tissue from your liver. A pathologist will examine the tissue under a microscope.
During a liver biopsy, a doctor will take a piece of tissue from your liver. A pathologist will examine the tissue under a microscope.Treatment
How do doctors treat NAFLD?
Doctors recommend weight loss to treat nonalcoholic fatty liver disease, or NAFLD (also referred to as metabolic dysfunction-associated steatotic liver disease, or MASLD). Weight loss can reduce fat in the liver. Weight loss can also reduce inflammation and fibrosis—or scarring—in the liver due to nonalcoholic steatohepatitis, or NASH (also referred to as metabolic dysfunction-associated steatohepatitis, or MASH).
If you are overweight or have obesity, losing weight by making healthy food choices, limiting portion sizes, and being physically active can improve NAFLD—either NAFL or NASH. Losing at least 3% to 5% of your body weight can reduce fat in the liver.5 You may need to lose up to 7% to 10% of your body weight to reduce liver inflammation and fibrosis.5 Physical activity alone, even without weight loss, is also beneficial.
Doctors recommend gradually losing weight to improve NAFLD. Rapid weight loss and malnutrition can make liver disease worse.
 If you are overweight or have obesity, losing weight can improve NAFLD.
If you are overweight or have obesity, losing weight can improve NAFLD.Medicines
No medicines have been approved to treat NAFLD—either NAFL or NASH. However, researchers are studying medicines that may improve these conditions.
For safety reasons, talk with your doctor before using dietary supplements, such as vitamins, or any complementary or alternative medicines or medical practices. Some herbal remedies can actually damage your liver.
How do doctors treat the complications of NASH?
If NASH leads to cirrhosis, doctors can treat many complications of cirrhosis with medicines, minor medical procedures, and surgery. People with liver failure or liver cancer may need a liver transplant to restore health.
How can I prevent NAFLD?
You may be able to prevent NAFLD by being physically active regularly, eating a healthy diet, limiting your portion sizes, and maintaining a healthy weight.
References
Eating, Diet, & Nutrition
How can my diet help prevent or treat NAFLD?
If you don’t have nonalcoholic fatty liver disease, or NAFLD (also referred to as metabolic dysfunction-associated steatotic liver disease, or MASLD), you may be able to prevent the condition by eating a healthy diet, limiting your portion sizes, and maintaining a healthy weight.
If you have NAFLD, your doctor may recommend gradually losing weight if you are overweight or have obesity.
Your doctor may suggest changes to your diet such as
- limiting your intake of fats, which are high in calories and increase your chance of developing obesity.
- replacing saturated fats and trans fats in your diet with unsaturated fats, especially omega-3 fatty acids, which may reduce your chance of heart disease if you have NAFLD.
- eating more low-glycemic index foods—such as most fruits, vegetables, and whole grains. These foods affect your blood glucose less than high-glycemic index foods, such as white bread, white rice, and potatoes.
- avoiding foods and drinks that contain large amounts of simple sugars, especially fructose. Fructose is found in sweetened soft drinks, sports drinks, sweetened tea, and juices. Table sugar, called sucrose, is rapidly changed to glucose and fructose during digestion and is therefore a major source of fructose.
If you have NAFLD, you should minimize alcohol use, which can further damage your liver.
Clinical Trials
The NIDDK conducts and supports clinical trials in many diseases and conditions, including liver diseases. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for NAFLD?
Clinical trials—and other types of clinical studies —are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help doctors and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of nonalcoholic fatty liver disease, or NAFLD (also referred to as metabolic dysfunction-associated steatotic liver disease, or MASLD).
- new treatments for NASH (also referred to as metabolic dysfunction-associated steatohepatitis, or MASH)
- how genes may increase the risk for NAFLD
- how liver diseases, such as NAFLD, develop and progress over time
Find out if clinical studies are right for you.
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical studies for NAFLD are looking for participants?
You can view a filtered list of clinical studies on NAFLD that are federally funded, open, and recruiting at ClinicalTrials.gov. You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe. Always talk with your health care provider before you participate in a clinical study.
What have we learned about NAFLD from NIDDK-funded research?
The NIDDK has supported many research projects to learn more about NAFLD and NASH. For example, the NIDDK’s NASH Clinical Research Network (NASH CRN) has conducted studies to advance understanding of the causes, development, complications, and treatment of NASH in children and adults. NASH CRN studies have included
- Pioglitazone or Vitamin E for NASH Study (PIVENS). Researchers found that a daily dose of the natural form of vitamin E—the type of vitamin E that comes from food sources and is not synthetic (laboratory-made)—improved NASH in study participants overall. Pioglitazone also improved some features of NASH, although researchers couldn’t prove that the improvements did not occur randomly. Many study participants taking pioglitazone gained weight, and many participants did not improve from either treatment. More research is needed to determine whether treatment with vitamin E or pioglitazone causes long-term risks.
- Treatment of Nonalcoholic Fatty Liver Disease in Children (TONIC) trial. The TONIC trial found that the natural form of vitamin E—the type of vitamin E that comes from food sources and is not synthetic (laboratory-made)—improved the most severe form of fatty liver disease in some children. More research is needed to determine whether treatment with vitamin E causes long-term risks.
- The Farnesoid X Receptor Ligand Obeticholic Acid in NASH Treatment Trial (FLINT). FLINT found that obeticholic acid (OCA) treatment was associated with improved liver function in people with NASH. OCA was also associated with increases in itching and total cholesterol. These results led to a large worldwide study that is still being evaluated to determine whether OCA is a safe and effective treatment for NASH and to fully understand how OCA affects cholesterol.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
NIDDK would like to thank:
Brent A. Tetri, M.D., Saint Louis University

