Interstitial Cystitis (Bladder Pain Syndrome)
Return to Overview PageDefinition & Facts
In this section:
- What is IC?
- How common is IC?
- Who is more likely to have IC?
- What other health problems do people with IC have?
- What are the complications of IC?
What is IC?
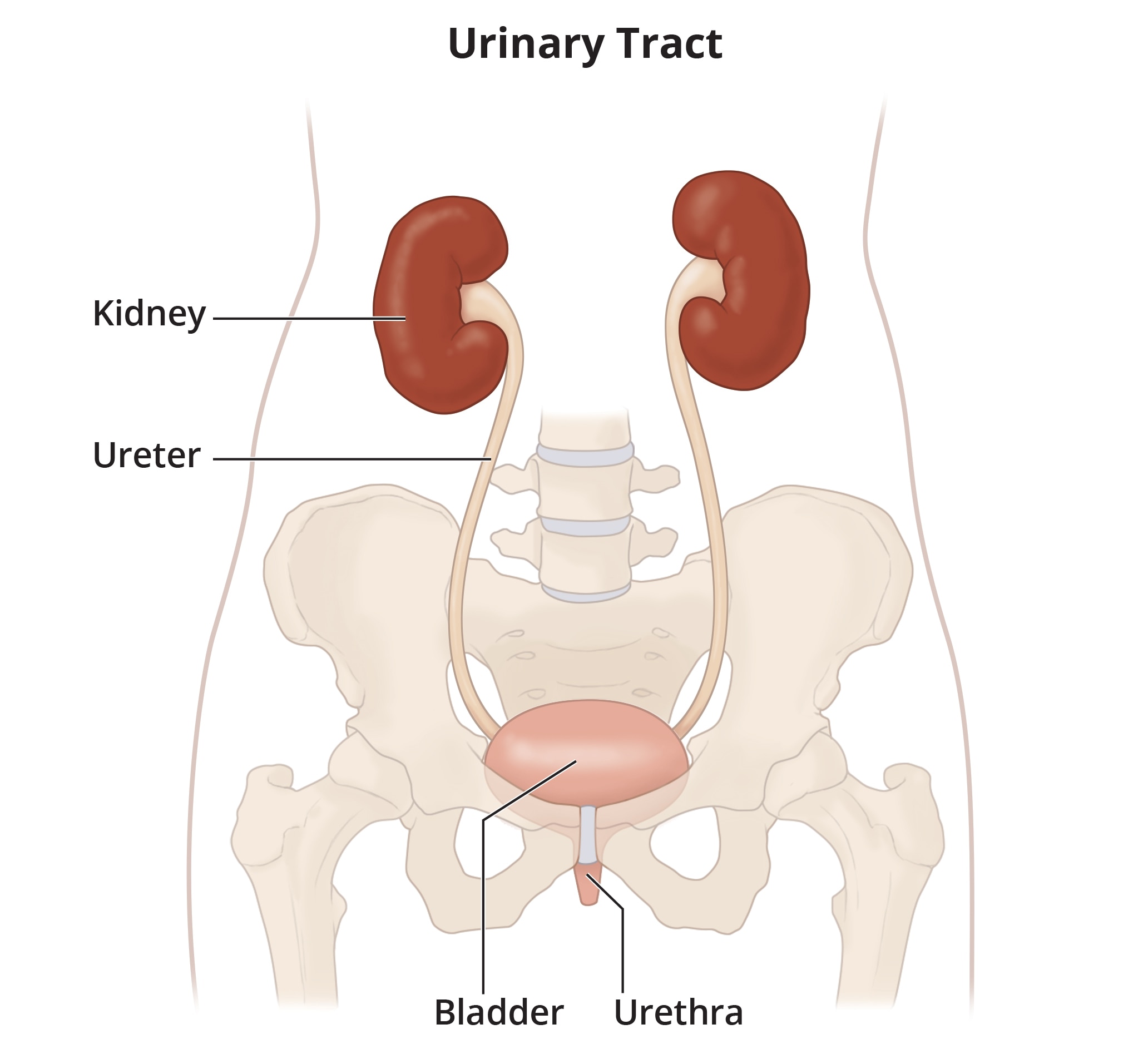
Interstitial cystitis (IC) is a chronic, or long-lasting, condition in which there is pain in the bladder. This pain usually gets worse as your bladder fills and gets better after you urinate. You may also feel pain in the groin and pelvic floor muscles. Symptoms of IC may be different among people. For example, some people feel mild discomfort, pressure, or tenderness in the pelvic area. Other people may have intense bladder pain or struggle with urinary urgency or urinary frequency.
Severe IC symptoms can affect your quality of life. You may feel like you can’t exercise or leave your home because you must use the bathroom too often. If sex is painful, you may worry about your relationship.
Working with health care professionals, such as a urologist or urogynecologist and a pain specialist, may help improve your IC symptoms.
Does IC have another name?
IC is also called bladder pain syndrome.
How common is IC?
IC is common. Between 4 and 12 million people in the United States may have IC.1 Experts don’t know the exact number because IC can be mistaken for other conditions.
Who is more likely to have IC?
IC is more common in women than men. IC can occur at any age, but it is more common in adults.
Some research suggests that women who experienced trauma as children may be more likely to develop IC.2
What other health problems do people with IC have?
People with IC are more likely to have
- other chronic pain conditions, such as fibromyalgia, vulvodynia, migraine, and chronic fatigue syndrome
- gastrointestinal or gastroesophageal disorders, such as irritable bowel syndrome and gastroesophageal reflux disease
- allergies
- autoimmune diseases
- mental health issues, such as depression and anxiety
Some studies show that women with IC experience these conditions more often than men with IC.3
What are the complications of IC?
Reduced physical and social activity
Physical activity is important for overall health. The symptoms of IC—such as urgency, frequency, and pain—may interfere with physical and social activity. Not getting enough of these activities may affect your quality of life.
Talk with your health care professional if your IC symptoms make it hard for you to be active.
Sleep loss
People with IC may struggle with sleep loss. You may not get enough sleep because of chronic pain. You may need to urinate several times during the night, which keeps you up. When you don’t get enough sleep, this can lead to other physical and mental health problems.
Talk with your health care professional if your IC symptoms make it hard for you to get enough sleep.
Intimacy problems
People with chronic pelvic pain—or vulvodynia—often have pain during sex, which can affect relationships and self-image. Sometimes sex can increase bladder pain attacks, also called symptom flares.
Problems with sex may cause people to avoid intimacy with their partners. These problems could lead to depression and guilt.
Pain during medical exams
Medical tests such as pelvic exams and Pap smear tests often are painful if you have IC. These tests may be more painful if you have spasms in your pelvic floor muscles. Don’t avoid these tests. Talk with your health care professional about how to make pelvic exams and Pap smear tests more comfortable and how often you should have them.
 Talk with your health care professional if your IC symptoms make it difficult for you to be active.
Talk with your health care professional if your IC symptoms make it difficult for you to be active.References
Symptoms & Causes
What are the symptoms of IC?
Interstitial cystitis (IC) symptoms vary among people. Symptoms may be mild or severe and can even change over time. Your symptoms may go away with treatment, a change in what you eat, or without a clear reason. Even if your symptoms go away, they may return after days, weeks, months, or even years.
Symptoms may include
- discomfort, pressure, or tenderness in the lower abdomen and pelvic area
- frequent urination, or needing to urinate more often than what’s normal for you
- pain in the bladder that worsens until you urinate and then improves for a little while
- pain during sex due to spasms in your pelvic floor muscles
- urinary urgency—with or without pain—before your bladder has time to fill
What causes IC?
Researchers aren’t sure exactly what causes IC. Some experts believe IC is caused by inflammation in the body. Your IC may feel worse when symptoms flare up. Certain factors may trigger symptom flares, including
- allergies or changes in the seasons or weather
- certain foods and drinks, skipping meals, or not drinking enough liquids to stay hydrated
- a urinary tract infection or holding urine for too long
- items that may cause irritation, such as laundry detergent, pool chemicals, toilet paper, and tight clothing
- physical activities that involve the pelvic floor, such as pushing or lifting heavy objects, bumpy movements, standing for a long time, and having sex
- stress and menstruation, which affect your hormones
 Your health care professional will discuss your IC symptoms with you.
Your health care professional will discuss your IC symptoms with you.If you know what makes your symptoms flare up, you may want to avoid them. Talk with your health care professional about factors that affect your health—like taking your prescribed medicines, having medical tests, or sex—if these cause symptom flares and make your IC feel worse.
Diagnosis
How do health care professionals diagnose IC?
Health care professionals diagnose interstitial cystitis (IC) by ruling out other conditions with similar symptoms. They will use your medical history, a physical exam, and lab and other tests to help diagnose IC. Your health care professional will ask questions about your symptoms and may have you keep a voiding log, also known as a bladder diary.
Medical history
A health care professional will ask
- if you have a history of health problems related to IC
- questions about your symptoms
- other questions to help find the cause of your bladder problems
Physical exam
Your health care professional will do a regular physical exam. To check your pelvic floor muscles, your health care professional may also do a
- pelvic exam if you are female
- digital rectal exam if you are male
Bladder diary
Your health care professional may ask you to keep a voiding log, also known as a bladder diary. A bladder diary will help you record the amount of liquids you drink and how much urine you pass.
What tests do health care professionals use to diagnose IC?
Health care professionals may use urinalysis, urine culture, and other tests to help diagnose IC or to rule out other conditions with similar symptoms.
Lab tests
Urinalysis
Urinalysis checks your urine sample for blood in the urine and white blood cells. Your body produces white blood cells when it is fighting an infection caused by bacteria.
Urine culture
Urine culture identifies some common types of bacteria in your urine. Bacterial infections, such as urinary tract infections, can be treated with antibiotics.
Other tests
Your health care professional may order tests to rule out other conditions or help make decisions about treating your IC, such as
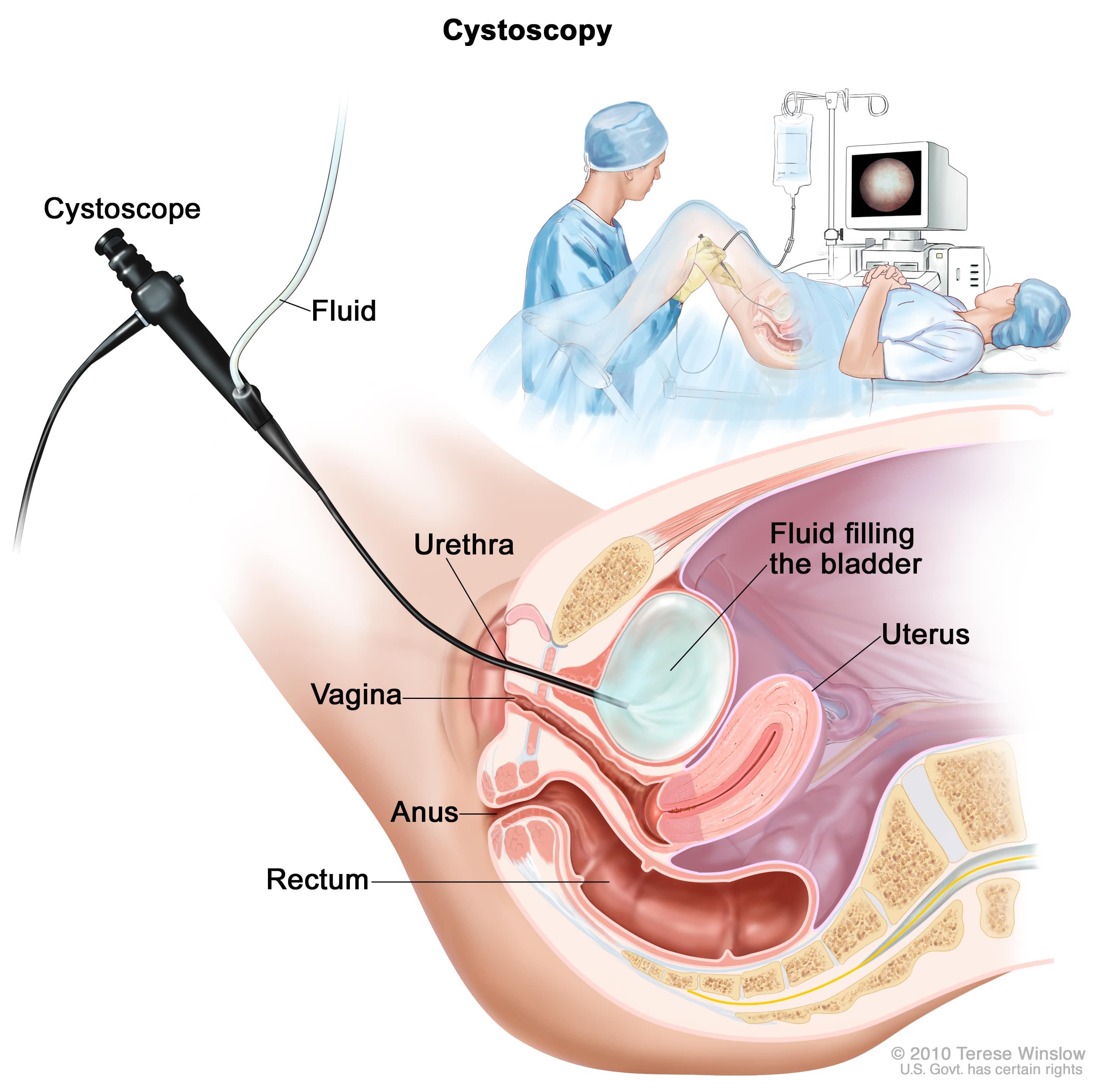
- cystoscopy to look inside the urethra and bladder
- urodynamic testing to measure how well parts of your urinary tract are storing and releasing urine
Treatment
How do health care professionals treat IC?
Health care professionals treat interstitial cystitis (IC) in different ways. They will work with you to determine what treatment reduces or stops your symptoms. Your care plan may include
- lifestyle changes
- bladder training
- physical therapy
- medicines
- neuromodulators
- bladder procedures
- surgery
While you try a treatment, your health care professional may ask you to fill out a form called a symptom scale. The symptom scale asks questions about how you feel. Your answers will help your health care professional understand how you respond to treatment. You may have to try several different treatments before you find what works best for you.
Lifestyle changes
Making changes to your daily life could help relieve IC symptoms.
Adjust what you eat and drink
Certain foods or drinks may seem to cause your symptoms to flare up. Avoiding these foods or drinks may reduce symptom flares. Keeping a food journal can help you identify which foods or drinks to avoid.
Stay hydrated
Staying hydrated is good for your body and your bladder. Talk with a health care professional about the amount of liquids that is right for you based on your health, activity level, and the climate where you live.
Quit smoking
If you smoke cigarettes, quitting smoking can reduce irritation to your bladder and improve your health overall. No matter how long or how much you have smoked, quitting smoking greatly benefits your health.
Be physically active
Activities like walking or gentle stretching exercises may help relieve your IC symptoms.
Reduce stress
Stress can impact your body in many ways. If you feel stressed, try relaxation techniques and other activities that may soothe you. A simple way to relax is deep breathing, which you can do anywhere.
Build a support system
The emotional support of family, friends, and people with IC can help you cope. Sharing your experience and becoming involved with others could help you to feel empowered and better overall.
Bladder training
A health care professional may recommend you try bladder training. Bladder training can help your bladder hold more urine, reduce pain and urgency, and help you to go to the bathroom less often.
Physical therapy
If you have IC symptoms or spasms in your pelvic floor muscles, you may be referred to a physical therapist who specializes in pelvic floor problems. The therapist will help you stretch tight pelvic floor muscles and keep them relaxed. If you have IC symptoms, you should avoid pelvic floor strengthening exercises, such as Kegel exercises, unless you are working with a physical therapist.
Medicines
If you have mild bladder pain, health care professionals may suggest over-the-counter pain relievers. They may prescribe other medicines if lifestyle changes, bladder training, physical therapy, and over-the-counter medicines don’t relieve your IC symptoms.
All medicines, even over-the-counter medicines, may cause side effects. Always talk with your health care professional before taking any medicines or supplements.
Neuromodulators
Though neuromodulators—or electric nerve stimulators—are not FDA-approved for IC, your health care professional may recommend one if other treatments for your symptoms don’t work. You can wear some neuromodulators outside on your body. There are other neuromodulators that a health care professional will place inside your body. Neuromodulators send mild electrical pulses to nerves to reduce pain and urinary frequency and urgency.
Bladder procedures
Bladder instillation
Bladder instillation, also called bladder wash or bath, may help relieve IC symptoms. A health care professional guides a catheter into your bladder and slowly adds a liquid medicine. You will keep the liquid medicine in your bladder for a little while and then release it. Your health care professional will recommend how often you should have this treatment. You may need several treatments before you feel better.
Bladder stretching
Bladder stretching, also called hydrodistention, may increase how much liquid your bladder can hold. A health care professional will first give you anesthesia to help you fall asleep and then stretch your bladder by filling it with water. Stretching may relieve bladder pain for a short time.
Botox
Though botulinum toxin type A, also called Botox, is not FDA-approved for IC, your health care professional may suggest using it if your symptoms do not go away with other treatments. Botox may help block the nerves in the bladder that cause pain and reduce pelvic floor muscle spasms. A health care professional will inject Botox directly into your bladder. You may need to repeat the number of Botox injections to relieve your IC pain long term.
Electrocauterization
Electrocauterization may help relieve the symptoms of Hunner lesions, a type of IC. The treatment uses an electric current to create heat. The heat is then used to burn, or cauterize, Hunner lesions in the bladder. Many patients with Hunner lesions feel relief from pain after this treatment. Sometimes, you may need more than one electrocauterization treatment.
Surgery
People rarely need surgery to treat IC. If you’ve tried all other options and your pain remains severe, you and your health care professional may consider surgery to enlarge or remove the bladder. However, these surgeries have a lot of risks and do not always cure the pain from IC.
Eating, Diet, & Nutrition
Can changing what I eat and drink improve my IC symptoms?
Some research suggests your diet may affect interstitial cystitis (IC) symptoms.4 Certain foods and drinks may cause your symptoms to get worse—called symptom flares. Learning what foods and drinks cause your symptom flares and taking steps to avoid them may help you feel better. Staying hydrated may also help improve your symptoms.
What types of foods and drinks could make IC worse?
Some people with IC find that certain foods or drinks cause symptom flares, such as
- citrus juices and drinks, such as orange and grapefruit juices
- coffee, tea, soda, and alcohol
- high-acid foods, such as tomatoes and tomato-based sauces
- hot and spicy foods
- artificial sweeteners, or sweeteners not found naturally in foods and drinks
- chocolate
- monosodium glutamate, or MSG, a food additive
 Some research suggests there may be a relationship between diet and IC symptoms.
Some research suggests there may be a relationship between diet and IC symptoms.How do I learn which foods and drinks make my IC worse?
A food diary can help you find out which foods and drinks cause your symptom flares. For example, the diary might show that you have symptom flares after you eat tomatoes or drink orange juice. When you know what foods and drinks trigger your symptom flares, you can avoid them.
Consider working with a registered dietitian, if possible, to create an eating plan for your individual needs. You can find a registered dietitian online through the Academy of Nutrition and Dietetics or through your health care professional. A dietitian can create a custom meal plan for you.
Reference
Clinical Trials
NIDDK conducts and supports clinical trials in many diseases and conditions, including urologic diseases. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for IC?
Clinical trials—and other types of clinical studies—are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help doctors and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of interstitial cystitis (IC), such as
- new, non-drug treatments for IC
- the relationship between IC and the gut microbiome
- how to target treatments for IC based on symptoms
Find out if clinical studies are right for you.
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical studies for IC are looking for participants?
You can view a filtered list of clinical studies on interstitial cystitis that are federally funded, open, and recruiting at ClinicalTrials.gov. You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe for you. Always talk with your health care provider before you participate in a clinical study.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
NIDDK would like to thank:
J. Quentin Clemens, M.D., University of Michigan

