Exocrine Pancreatic Insufficiency (EPI)
Return to Overview PageDefinition & Facts
In this section:
What is EPI?
Exocrine pancreatic insufficiency (EPI) is a condition in which your small intestine can’t digest food completely because of problems with digestive enzymes from your pancreas. EPI often develops slowly, over many years.
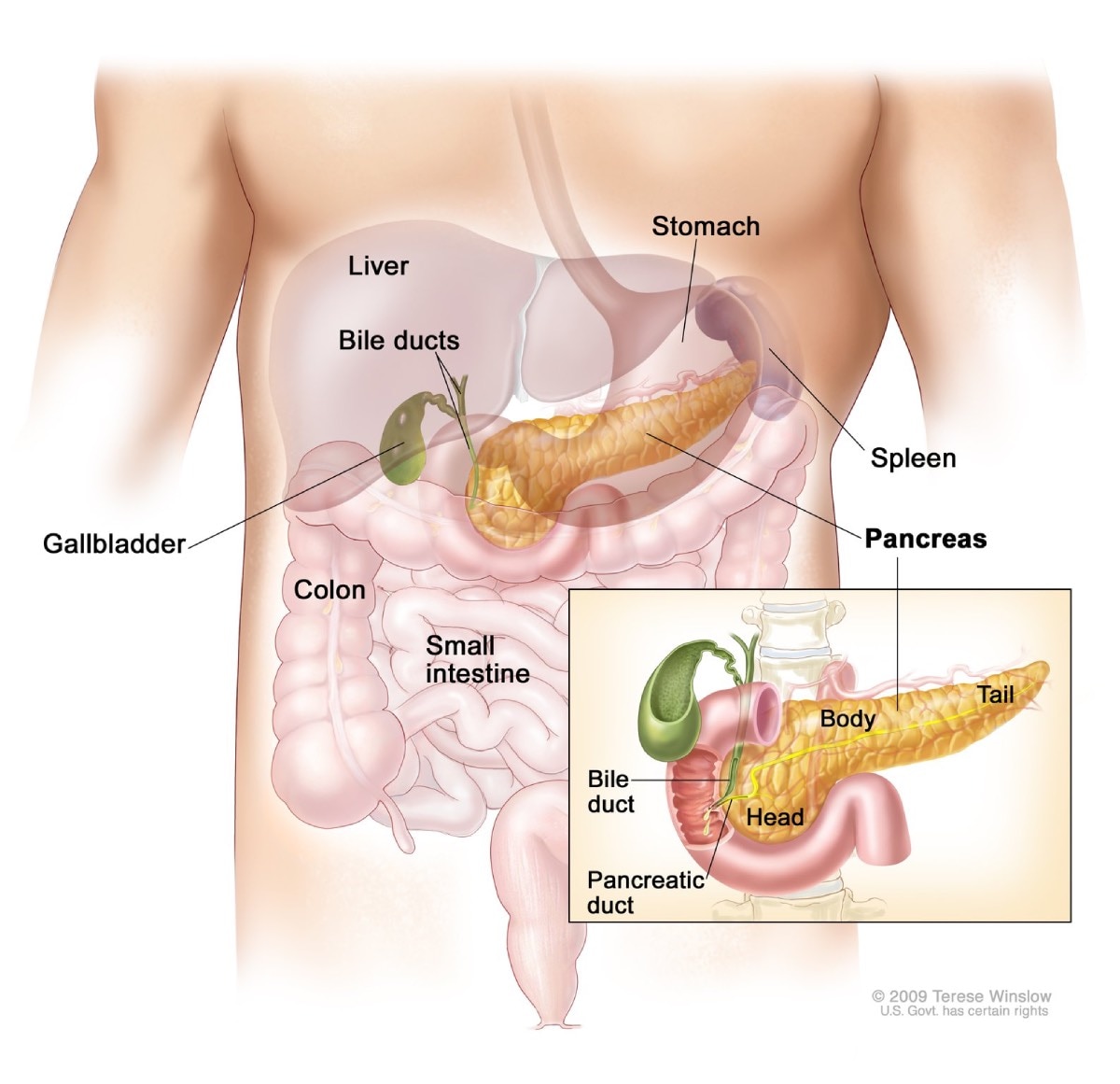
The pancreas is a large gland behind your stomach. The pancreas is both
- an endocrine gland that makes hormones
- an exocrine gland that makes digestive juice containing enzymes
The pancreas delivers the digestive juice to the small intestine through a single duct. In the small intestine, the enzymes from the pancreas help digest food, breaking down carbohydrates, fats, and proteins.
You may develop EPI if
- the amount of enzymes your pancreas makes is severely reduced
- not enough enzymes reach your small intestine
- other problems prevent the enzymes from mixing with food or otherwise working well
How common is EPI?
EPI is rare. However, problems with enzymes from the pancreas occur more often in people with certain health conditions.
Although study results vary, experts think problems with enzymes from the pancreas may occur in1
- 30% to 90% of people with chronic pancreatitis
- 80% to 90% of people with cystic fibrosis
Less commonly, problems with enzymes in the pancreas may occur in people who have
- pancreatic cancer that has not been removed by surgery
- type 1 diabetes or type 2 diabetes
- inflammatory bowel disease
- untreated celiac disease
- surgery of the pancreas or upper gastrointestinal tract
- Sjogren’s syndrome
- a history of smoking or drinking alcohol
Who is more likely to have EPI?
People who have advanced pancreatic diseases are more likely to develop EPI. For example, EPI is more common in people who have
- chronic and acute pancreatitis
- cystic fibrosis
- pancreatic cancer
- surgery of the pancreas or upper gastrointestinal tract
What are the complications of EPI?
In EPI, the small intestine doesn’t digest food as it should and may not absorb enough nutrients—a condition called malabsorption. EPI and malabsorption can lead to complications such as
- malnutrition
- low levels of fat-soluble vitamins A, D, E, and K in the body
- low bone mass, called osteopenia, and osteoporosis
- problems with growth in children
- weakness of the immune system
- increased risk of cardiovascular events, such as heart attack and stroke
Reference
Symptoms & Causes
What are the symptoms of EPI?
Symptoms of exocrine pancreatic insufficiency (EPI) may include
- bloating
- cramps, discomfort, or pain in the abdomen
- diarrhea
- loose, greasy, bad-smelling stools
- passing excess gas, or flatulence
- weight loss
In rare cases, EPI may lead to problems seeing at night or problems with your bones, such as low bone mass or osteoporosis.
What causes EPI?
 Symptoms of EPI may include cramps, discomfort, or pain in the abdomen.
Symptoms of EPI may include cramps, discomfort, or pain in the abdomen.
Common causes of EPI include
- chronic and acute pancreatitis
- cystic fibrosis
- pancreatic cancer
- surgery of the pancreas or upper gastrointestinal tract
Less common causes of EPI include
- diabetes—type 1 and type 2
- untreated celiac disease
- inflammatory bowel disease, including Crohn’s disease and ulcerative colitis
- HIV
- rare genetic disorders, such as Shwachman-Diamond syndrome and Johanson-Blizzard syndrome
- Zollinger-Ellison syndrome
Diagnosis
How do doctors diagnose EPI?
To diagnose exocrine pancreatic insufficiency (EPI), your doctor will ask about your medical and family history, perform a physical exam, and order tests.
Medical and family history
To help diagnose EPI, your doctor will ask about your
- symptoms
- history of diseases and conditions that may cause EPI
- family history of pancreatitis
- history of excessive alcohol consumption, which may increase your chance of developing chronic pancreatitis
- history of smoking, which may increase your chance of developing pancreatitis and pancreatic cancer
 To help diagnose EPI, your doctor will ask about your symptoms and medical and family history.
To help diagnose EPI, your doctor will ask about your symptoms and medical and family history.Physical exam
During a physical exam, your doctor may
- examine your body for signs of weight loss or malnutrition
- check your abdomen for swelling
- listen to sounds within your abdomen using a stethoscope
- tap on your abdomen checking for tenderness or pain
What tests do doctors use to diagnose EPI?
Doctors most often order stool tests, blood tests, and sometimes pancreatic function tests to diagnose EPI. Doctors may order additional tests to check for diseases that can cause EPI, if the cause is unknown.
Stool tests
Stool elastase test, also called fecal elastase-1 or FE-1 test, is the most commonly used stool test. Low levels of FE-1 in the stool may be a sign of EPI. Your doctor will give you a container for catching and holding a stool sample. You should provide a solid or semisolid stool sample for this test. You will receive instructions on where to send or take the kit for testing.
Blood tests
A health care professional will take a blood sample from you and send the sample to a lab. Doctors may use blood tests to check for low levels of fat-soluble vitamins and minerals or other signs of malnutrition.
Pancreatic function test
Your doctor may order a pancreatic function test to measure how your pancreas responds to secretin, a hormone made by the small intestine. The test measures pancreatic fluid instead of pancreatic enzymes and may not accurately diagnose EPI. This test is done only at some centers in the United States.
During a pancreatic function test, health care professionals give you intravenous (IV) secretin and insert a tube through your nose and into your small intestine. Health care professionals will collect fluid samples with the tube and send the samples to a lab for analysis.
In some cases, doctors use upper gastrointestinal (GI) endoscopy to perform part or all of this test.
Treatment
How do doctors treat EPI?
Doctors treat exocrine pancreatic insufficiency (EPI) with pancreatic enzyme replacement therapy (PERT) and lifestyle changes.
Doctors may recommend additional treatments for the diseases or conditions that cause EPI.
PERT
To treat EPI, doctors typically prescribe PERT. PERT involves taking pills that contain pancreatic enzymes. PERT can improve your symptoms and help you get enough nutrients from what you eat and drink.
PERT is taken during meals or snacks to help your small intestine with digestion. Follow your doctor’s instructions about how and when to take PERT.
 Taking PERT during meals or snacks can help your body with digestion.
Taking PERT during meals or snacks can help your body with digestion.Lifestyle changes
Lifestyle changes can also help treat EPI. Your doctor may recommend you
- avoid alcohol
- make changes to eating, diet, and nutrition
- quit smoking
How do doctors prevent and treat complications of EPI?
If you have EPI, your doctor may order tests to check for complications, such as
- malnutrition
- low levels of fat-soluble vitamins A, D, E, and K
- low bone mass
Doctors may recommend you take dietary supplements of fat-soluble vitamins or other nutrients to help prevent or treat these complications.
For safety reasons, talk with your doctor before using dietary supplements, such as vitamins, or any complementary or alternative medicines or medical practices.
Eating, Diet, & Nutrition
How does EPI affect nutrition?
If you have exocrine pancreatic insufficiency (EPI), your small intestine can’t digest food normally because of problems with enzymes produced by the pancreas. When the small intestine doesn’t digest food as it should, it may not absorb enough nutrients—a condition called malabsorption.
Malabsorption can lead to
- malnutrition
- low levels of fat-soluble vitamins A, D, E, and K
- low bone mass, called osteopenia, and osteoporosis
- problems with growth in children
EPI treatment can help correct malabsorption.
What should I eat if I have EPI?
Your doctor may refer you to a registered dietitian to help you create a healthy meal plan. Check on the cost of a dietitian’s services and whether your health insurance may pay for some or all of these services.
Your doctor or dietitian may recommend changes to eating and nutrition, such as
- eating small, frequent meals
- taking pancreatic enzyme replacement therapy (PERT) when you eat
- taking dietary supplements for low levels of fat-soluble vitamins or other nutrients
- avoiding alcohol and quitting smoking
Your doctor or dietitian may recommend additional changes to eating, diet, and nutrition to treat the cause of EPI.
 Your doctor or dietitian may recommend you eat small, frequent meals.
Your doctor or dietitian may recommend you eat small, frequent meals.Clinical Trials
The NIDDK conducts and supports clinical trials in many diseases and conditions, including digestive diseases. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for EPI?
Clinical trials—and other types of clinical studies—are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help doctors and researchers learn more about disease and improve health care for people in the future.
Researchers are conducting clinical studies to better understand digestive diseases, such as exocrine pancreatic insufficiency (EPI). For example, researchers are studying ways to improve diagnosis and treatment of EPI and the diseases that cause EPI.
Find out if clinical studies are right for you.
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical studies for EPI are looking for participants?
You can view a filtered list of clinical studies on EPI that are federally funded, open, and recruiting at ClinicalTrials.gov. You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the NIH does not review these studies and cannot ensure they are safe. Always talk with your health care provider before you participate in a clinical study.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
The NIDDK would like to thank:
Christopher E. Forsmark, M.D., University of Florida College of Medicine; Suresh T. Chari, M.D., University of Texas MD Anderson Cancer Center