Gastrointestinal Bleeding
Return to Overview PageDefinition & Facts
What is GI bleeding?
Gastrointestinal (GI) bleeding is any type of bleeding that starts in your GI tract, also called your digestive tract. GI bleeding is a symptom of a complication of another disease or condition.
 The digestive tract.
The digestive tract.
What are the types of GI bleeding?
GI bleeding is grouped by where in the GI tract the bleeding takes place.
- Upper GI bleeding occurs in the esophagus, stomach, or the upper duodenum. The duodenum is the first part of the small intestine.
- Small bowel GI bleeding occurs in the jejunum or ileum in the middle and lower small intestine.
- Lower GI bleeding occurs in the large intestine or the anus.
GI bleeding can be acute or chronic.
- Acute GI bleeding begins suddenly and may sometimes be severe.
- Chronic GI bleeding is light bleeding that can last a long time or may come and go.
How common is GI bleeding?
In the United States, GI bleeding leads to more than 1.5 million health care visits1 and half a million hospital stays each year.2 In addition, GI bleeding occurs in people in the hospital for other reasons in over half a million hospitalizations each year.1 Upper GI bleeding is more common than lower GI bleeding, which is more common than small bowel bleeding.
Who is more likely to have GI bleeding?
Anyone can have GI bleeding. The chance of having GI bleeding increases with age.3,4,5
You are also more likely to have GI bleeding if you have a disease or condition that can cause GI bleeding.
 The chance of having GI bleeding increases with age.
The chance of having GI bleeding increases with age.
References
Symptoms & Causes
What are the symptoms of GI bleeding?
Gastrointestinal (GI) bleeding symptoms depend on the type of GI bleeding you have. If you have symptoms of acute or severe GI bleeding, seek medical help right away.
Acute GI bleeding
Acute bleeding begins suddenly and can sometimes be severe. You may notice symptoms, such as
- black or tarry stool
- dark or bright red blood mixed with stool
- bright red blood in vomit
- vomit that looks like coffee grounds
Acute GI bleeding may have other symptoms, such as
- having cramps or pain in your abdomen
- fainting or feeling lightheaded or dizzy
- feeling tired
- having shortness of breath
If acute GI bleeding is severe, you could go into shock. Symptoms of shock include
- confusion or unconsciousness
- fast heart rate
- pale skin
- cold hands and feet
- sweating
Shock is life-threatening. If you have symptoms of shock, seek emergency medical help right away.
 Symptoms of acute GI bleeding may include feeling dizzy or fainting.
Symptoms of acute GI bleeding may include feeling dizzy or fainting.
Chronic GI bleeding
Chronic GI bleeding may cause you to have a small amount of blood in your stool. If the amount of blood is too small for you or your doctor to see, it is called occult bleeding. Doctors can order stool and blood tests to check for occult bleeding.
In some cases, chronic GI bleeding causes mild symptoms that come and go over time. In addition, you may have variable symptoms and notice that your stool is sometimes black and tarry or sometimes mixed with bright red blood.
Over time, chronic bleeding can cause anemia. Symptoms of anemia may include
- feeling tired
- pale skin
- shortness of breath
If the amount of bleeding suddenly increases, you may have symptoms of acute GI bleeding. If you have symptoms of acute GI bleeding, seek medical help right away.
What causes GI bleeding?
A variety of diseases and conditions can cause GI bleeding, and these vary by where in the GI tract the bleeding takes place.
Upper GI bleeding
Causes of upper GI bleeding include6
- peptic ulcers, sores on the lining of the stomach or duodenum that may bleed. The most common causes of peptic ulcers are Helicobacter pylori (H. pylori) infection and taking nonsteroidal anti-inflammatory drugs (NSAIDs)—such as aspirin, ibuprofen, and naproxen—and blood thinners.
- gastritis, which occurs when the stomach lining is inflamed or damaged. This condition may lead to shallow breaks or ulcers in the stomach lining that bleed. Causes of gastritis include H. pylori infection, taking NSAIDs and blood thinners, and drinking alcohol.
- esophagitis, inflammation in the esophagus that may lead to ulcers and bleeding. Esophagitis is often caused by gastroesophageal reflux disease.
- varices—enlarged veins—in the esophagus or stomach that can cause bleeding if the veins burst. Varices are most often related to cirrhosis.
- Mallory-Weiss tears, tears in the lower esophagus that can bleed. These tears are often caused by severe vomiting.
- benign tumors or cancer, which may occur in the esophagus or stomach. These abnormal growths can weaken the lining of the GI tract, exposing blood vessels and causing bleeding.
Small bowel bleeding
Causes of small bowel bleeding include7,8
- angiodysplasia, a condition in which blood vessels in the GI tract are abnormal or enlarged. These abnormal or enlarged blood vessels can become weak and bleed.
- inflammation in the small bowel, which may lead to erosions and ulcers and cause bleeding. Causes of small bowel inflammation include Crohn’s disease, NSAIDs, and infections.
- polyps, benign tumors, or cancer, which may occur in the small bowel. These abnormal growths can weaken the lining of the GI tract and cause bleeding.
Lower GI bleeding
Causes of lower GI bleeding include9
- diverticular disease, in which small pouches, or sacs, form and push outward through weak spots in the wall of your colon. Diverticular bleeding occurs when a small blood vessel within the wall of a pouch bursts.
- hemorrhoids, swollen and inflamed veins around your anus or in your lower rectum that may bleed, or anal fissures, small tears that also can cause itching, tearing, or bleeding in your anus.
- polyps, benign tumors, or cancer, which may occur in the colon or rectum. These abnormal growths can weaken the lining of the GI tract and cause bleeding.
- colitis, inflammation in the colon that may lead to ulcers and bleeding. Causes of colitis include lack of blood flow to the colon, inflammatory bowel disease (IBD)—such as ulcerative colitis or Crohn’s disease—and infections.
References
Diagnosis
How do doctors diagnose GI bleeding?
Your doctor will ask about your medical and family history and perform a physical exam. Doctors may also order tests to diagnose gastrointestinal (GI) bleeding, find out how severe the bleeding is, and find its cause.
Medical and family history
Your doctor may ask about your
- symptoms
- medicines, including any over-the-counter medicines you take, such as nonsteroidal anti-inflammatory drugs (NSAIDs)—including aspirin—and blood thinners
- medical history, including any history of GI bleeding or conditions that can cause GI bleeding
- family history, including any conditions that can cause GI bleeding
Physical exam
During a physical exam, your doctor may
- check your vital signs, including blood pressure, heart rate, and temperature
- press on your abdomen to feel for tenderness or masses
- use a stethoscope to listen to your heart and sounds within your abdomen
The physical exam may also include a digital rectal exam.
What tests do doctors use to diagnose GI bleeding?
Your doctor may order tests to help diagnose GI bleeding, find the source of bleeding, or find its cause. In some cases, doctors can both diagnose and treat GI bleeding at the same time.
Lab tests
To help diagnose GI bleeding and find the cause, doctors may order
- stool tests. A health care professional will give you a container for catching and storing the stool. You will receive instructions on where to send or take the container so the stool can be studied. Stool tests can show occult bleeding.
- blood tests. A health care professional will take a blood sample from you and send the sample to a lab. Blood tests can show how severe your GI bleeding is and whether you have anemia.
Endoscopy
Endoscopy tests help diagnose and find the cause of bleeding in the GI tract.
During an endoscopy, doctors use an endoscope—a long, flexible, narrow tube with a light and tiny video camera on one end—to view inside the GI tract. Doctors may take biopsies during endoscopy tests to help diagnose the cause of GI bleeding. In some cases, doctors can treat active GI bleeding or prevent further bleeding during an endoscopy.
Doctors may order several types of endoscopy tests, which include
- upper GI endoscopy to see inside your esophagus, stomach, and duodenum
- enteroscopy to see inside your small intestine
- colonoscopy to see inside your rectum and your entire colon
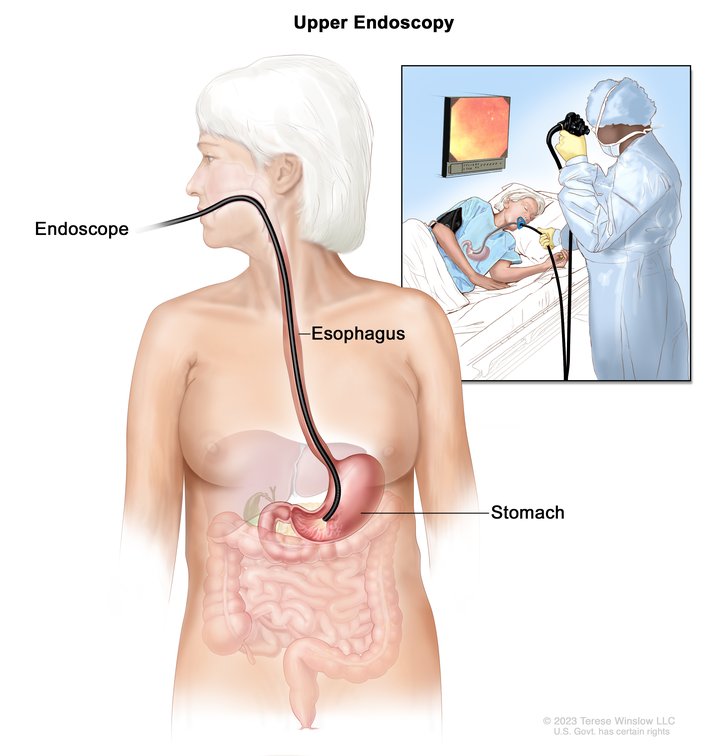 View full-sized image Doctors use endoscopy tests to help diagnose and treat bleeding in the GI tract.
View full-sized image Doctors use endoscopy tests to help diagnose and treat bleeding in the GI tract.
Capsule endoscopy
Capsule endoscopy tests check for GI bleeding in the small intestine, which is over 20 feet in length.
For a capsule endoscopy test, you swallow a capsule that contains a tiny camera, and you wear a device called a recorder. As the capsule passes through your GI tract, the camera records images and sends the images to the recorder. You will return the recorder to your doctor. Your doctor will review the images to check for active bleeding and find the cause and location of the bleeding. The capsule will leave your body during a bowel movement and can be flushed down the toilet.
Imaging tests
X-ray imaging tests can help find the source or cause of GI bleeding.
Doctors may order other imaging tests, such as
- computed tomography (CT) and CT angiography (CTA), which use a combination of x-rays and computer technology to create images
- radionuclide scanning, in which you receive an injection of a small amount of radioactive material, and a special camera takes pictures that highlight the radioactive material and show GI bleeding
Other imaging tests
Angiography
Angiography uses special dye and x-rays to see how your blood flows through your blood vessels. Doctors usually order this test for a person with GI bleeding if other tests haven’t been able to treat the bleeding.
A doctor inserts a catheter into your blood vessel, adds the dye, and then takes x-ray images. Doctors will analyze the images for signs of active GI bleeding. Doctors may be able to treat GI bleeding during an angiography.
Surgery
Doctors may recommend surgery to find the source and cause of GI bleeding if
- you have severe bleeding that doesn’t stop
- doctors can’t find the exact source or cause of GI bleeding with endoscopy or imaging tests
The surgery may be laparoscopic or open. During laparoscopic surgery, surgeons make small cuts in your abdomen and insert a laparoscope—a thin tube that has a tiny video camera and light attached—and other tools. In open surgery, surgeons make a larger cut to open your abdomen.
In some cases, doctors can diagnose and treat GI bleeding at the same time.
Treatment
How do doctors treat GI bleeding?
Treating gastrointestinal (GI) bleeding depends on how severe the bleeding is, its cause, and where in the GI tract the bleeding takes place. If you have symptoms of GI bleeding, seek medical help right away.
Medical treatments
Doctors may use medical treatments to stop GI bleeding, prevent further bleeding, or care for the problem that caused the bleeding. In some cases, doctors can diagnose and treat GI bleeding at the same time.
Endoscopy
Endoscopy procedures include upper GI endoscopy, enteroscopy, and colonoscopy. During an endoscopy, a doctor can insert tools through the endoscope to
- inject medicines into the bleeding site
- treat the bleeding site and surrounding tissue with an electric current to burn and seal the bleeding blood vessel
- apply a band or clip to close blood vessels that are bleeding
- spray a powder or gel to stop bleeding from a blood vessel
Angiography
During an angiography, a doctor inserts a catheter into your blood vessels. The doctor can inject medicines or other materials through the catheter to stop some types of bleeding.
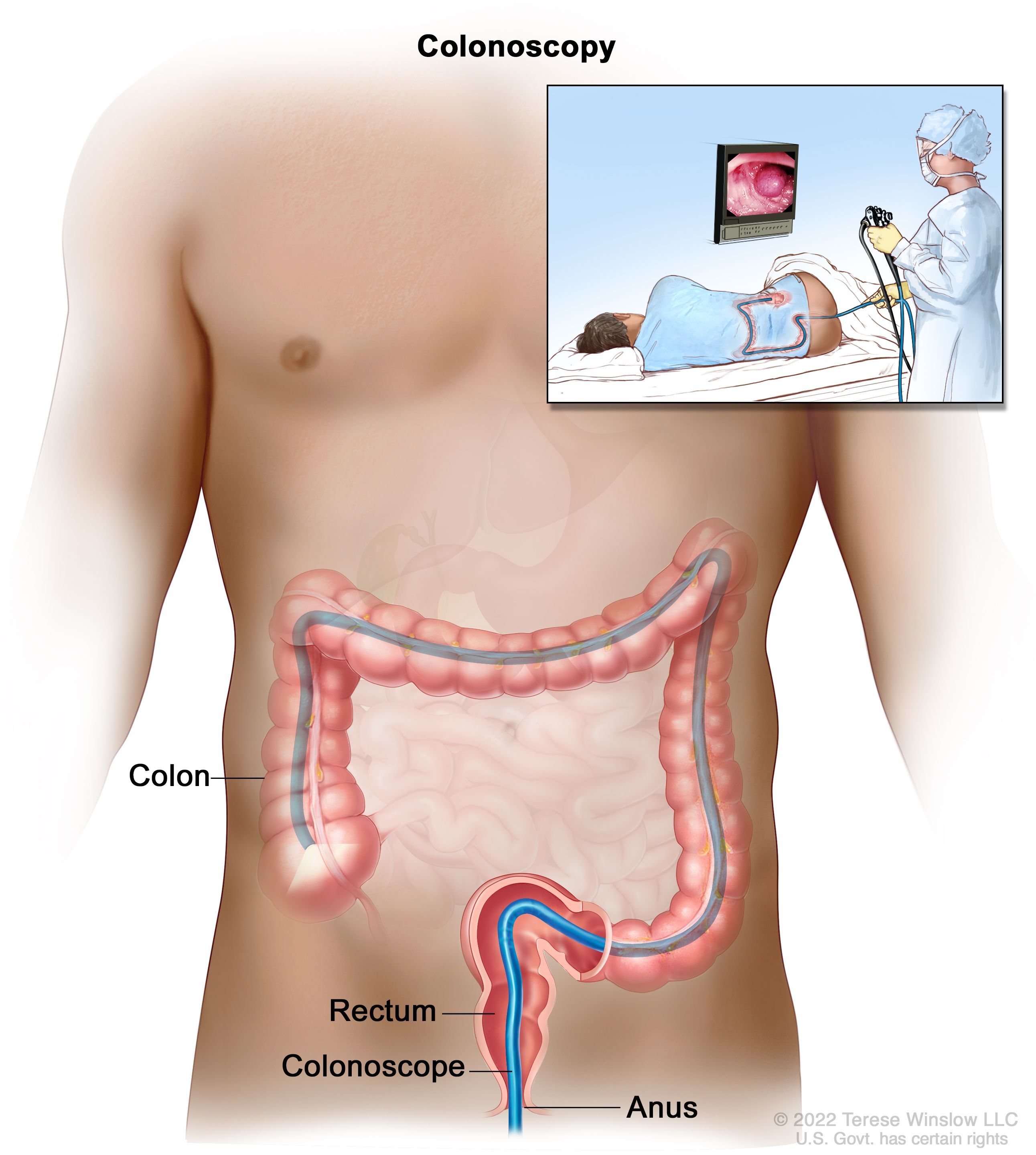 View full-sized image Doctors may use medical treatments, such as colonoscopy, to stop GI bleeding.
View full-sized image Doctors may use medical treatments, such as colonoscopy, to stop GI bleeding.
Medicines
Doctors may recommend medicines to treat some of the causes of GI bleeding, such as peptic ulcers, gastritis, and inflammatory bowel disease.
Surgery
If you have severe bleeding or bleeding that does not stop after other treatments, you may need surgery.
Doctors may recommend laparoscopic or open surgery to stop GI bleeding. During laparoscopic surgery, surgeons make small cuts in your abdomen and insert a laparoscope and other tools. In open surgery, surgeons make a larger cut to open your abdomen.
How can I prevent GI bleeding?
If you have a disease or condition that may cause GI bleeding, you can lower your risk of bleeding by following your doctor’s treatment plan.
Nonsteroidal anti-inflammatory drugs (NSAIDs), which are available over the counter and by prescription, may increase the chance of having GI bleeding. Some other medicines, when taken along with NSAIDs, can also increase the risk of bleeding.
Blood thinners may increase the chance of having GI bleeding or the severity of a GI bleed. The risk is higher in patients taking these medicines along with NSAIDs or aspirin and in those who have had GI bleeding in the past.
Talk with your doctor about the medicines you take, including over-the-counter medicines and supplements. In some cases, doctors may recommend changes to your medicines or prescribe a medicine to lower your GI bleeding risk.
Eating, Diet, & Nutrition
Can changes to my diet help prevent or treat GI bleeding?
Depending on the disease or condition that caused your gastrointestinal (GI) bleeding, your doctor may recommend changes to your diet or lifestyle to lower your chance of having future GI bleeding. For example, doctors may recommend
- avoiding medicines that can cause or worsen GI bleeding, such as nonsteroidal anti-inflammatory drugs (NSAIDS)
- increasing the amount of fiber in your diet if you have diverticular disease or hemorrhoids
- not drinking alcohol if you have esophageal varices due to cirrhosis
- quitting smoking, which may help prevent or treat a number of diseases, including peptic ulcers, diverticular disease, and gastroesophageal reflux disease
Clinical Trials
NIDDK conducts and supports clinical trials in many diseases and conditions, including digestive diseases. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for GI bleeding?
Clinical trials—and other types of clinical studies—are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help doctors and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of gastrointestinal (GI) bleeding, including
- new ways to find the source of GI bleeding
- improved treatments to stop GI bleeding
- strategies to prevent GI bleeding from recurring
Find out if clinical trials are right for you.
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical studies for GI bleeding are looking for participants?
You can view a filtered list of clinical studies on GI bleeding that are federally funded, open, and recruiting at ClinicalTrials.gov. You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, NIH does not review these studies and cannot ensure they are safe for you. Always talk with your health care provider before you participate in a clinical study.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
NIDDK would like to thank:
John Saltzman, M.D., Harvard Medical School
