Bladder Control Problems (Urinary Incontinence)
Return to Overview PageDefinition & Facts
In this section:
- What are bladder control problems?
- Do bladder control problems have another name?
- What are the types of bladder control problems?
- How common are bladder control problems?
- Who is more likely to develop bladder control problems?
- What are the complications of bladder control problems?
What are bladder control problems?
Bladder control problems are conditions that affect the way a person holds or releases urine. Accidental loss or leaking of urine, called urinary incontinence (UI), is one of the most common bladder control problems. UI is not a disease but a condition that may be related to another health problem or life event, such as prostate problems or pregnancy.
 Talk with a health care professional about how to manage your bladder control problem and lifestyle changes you can make.
Talk with a health care professional about how to manage your bladder control problem and lifestyle changes you can make.Bladder control problems can be a small annoyance or can greatly affect your quality of life. You may be too embarrassed or afraid to participate in activities because of these problems, or you may be unable to complete your normal routine. For example, you may lose urine while running or coughing, or you may leak urine before you can get to a toilet.
Bladder control problems are common. Proper treatment may improve your quality of life. Talk with a health care professional about urine leaks. Health care professionals—especially gynecologists, urologists, and geriatricians—often talk with people about bladder control problems. Health care professionals can help treat the problem or manage the symptoms by suggesting simple lifestyle changes. Caregivers may find help from a health care professional or a support group. The sooner you get help, the sooner UI may improve.
Do bladder control problems have another name?
Bladder control problems that cause urine to leak are also called urinary incontinence (UI), urine leakage, and urine loss.
What are the types of bladder control problems?
Types of bladder control problems are identified by their symptoms. The most common bladder control problems include
- stress incontinence
- urgency incontinence
- reflex incontinence
- overflow incontinence
- functional incontinence
- temporary incontinence
- bedwetting
Stress incontinence
Stress incontinence occurs when movement—coughing, sneezing, laughing, or physical activity—puts pressure on the bladder and causes urine to leak.
Urgency incontinence
Urgency incontinence occurs when you have a strong urge or need to urinate, and urine leaks before you can get to a toilet. Urgency incontinence is often referred to as overactive bladder. This type of incontinence happens when certain nerves and bladder muscles don’t work together to hold urine in the bladder, and the urine is released at the wrong time.
You can have urgency and stress incontinence at the same time, which is called mixed incontinence.
Reflex incontinence
With reflex incontinence, urine leaks without a warning or urge to urinate. This type of incontinence often happens when your bladder nerves are damaged and don’t “talk” to your brain correctly. During reflex incontinence, the bladder contracts, or reflexes, at the wrong time, causing urine to leak. Nerve damage from health conditions, such as multiple sclerosis NIH external link, or from trauma, such as a spinal cord injury NIH external link, are among the causes of reflex incontinence. Reflex incontinence is sometimes called “unaware” or “unconscious” incontinence.
Overflow incontinence
Overflow incontinence occurs when the bladder doesn’t empty all the way, causing too much urine to stay in the bladder. With overflow incontinence, urine leaks because the bladder becomes too full.
Functional incontinence
Functional incontinence occurs when a physical disability or barrier, or a problem speaking or thinking, prevents you from reaching the toilet in time. For example, a person in a wheelchair may not be able to get to a toilet in time, someone with arthritis NIH external link may have trouble unbuttoning his or her pants, or a person with Alzheimer’s disease NIH external link may not realize he or she needs time to get to the toilet.
Temporary incontinence
Temporary, or transient, incontinence lasts a short time due to a temporary situation, such as using a certain medicine or having an illness that causes leaking. For example, a urinary tract infection (UTI) or a bad cough may cause temporary incontinence.
Bedwetting
Bedwetting, also called nocturnal enuresis, doesn’t only occur in children. Some adults leak urine while sleeping for a variety of reasons. Certain medicines or drinking caffeine or alcohol at night can make it hard to sleep through the night without leaking urine. In some cases, the bladder can’t hold enough urine overnight. Lifestyle changes often can improve these symptoms.
Some people wet the bed because they don’t produce enough of a certain hormone at night, which could be a sign of diabetes insipidus. Other health problems, such as a UTI, kidney stones, congestive heart failure, chronic kidney disease, prostate enlargement, or obstructive sleep apnea NIH external link, can cause you to wet the bed or urinate frequently at night.
How common are bladder control problems?
Bladder control problems are common, especially in women. Researchers estimate that approximately half of all women experience UI.1 Women are more likely to develop UI during and after pregnancy, childbirth, and menopause NIH external link. These events and how the female urinary tract is built make UI more common in women than men. Although UI is common, it is not a routine part of being a woman or getting older.
As many as 1 in 3 men over the age of 65 may lose urine by accident, and approximately half of men who seek treatment for lower urinary tract symptoms experience UI.2,3 A man is more likely to develop UI with age because prostate problems occur more often with age.

Who is more likely to develop bladder control problems?
Factors that make you more likely to develop UI include
- being female
- being older—as you age, your urinary tract muscles weaken, making it harder to hold in urine
- life events, such as pregnancy, childbirth, and menopause in women and prostate problems in men
- health problems, such as diabetes, obesity, Parkinson’s disease NIH external link, multiple sclerosis, or long-lasting constipation
- smoking
- birth defects NIH external link that involve a problem with the structure of the urinary tract
Your health care professional can help find the cause of your bladder control problems and talk with you about your options for treatment.
You are more likely to have a particular type of UI if a family member has that same type of UI. For example, bedwetting often runs in families, and children may outgrow the problem at about the same age their parents did.
What are the complications of bladder control problems?
Reduced physical activity
Physical activity is important for overall health and may prevent further bladder control problems. However, some activities such as running, jumping, or brisk walking may cause some people with UI to leak. If you haven’t found a medicine or other treatment that’s right for you, or you want extra peace of mind, new incontinence briefs and pads are discreet and effective at absorbing leaks and controlling odor. New technology and designs can make these products more comfortable to wear and may give you the confidence to get moving again.
Talk with your health care professional if your bladder control problems are making it difficult for you to be active.
 Bladder problems don’t have to limit your activities. Getting help from a health care professional may keep you moving.
Bladder problems don’t have to limit your activities. Getting help from a health care professional may keep you moving.Emotional distress
Untreated bladder problems can upset your lifestyle. You may avoid activities you once enjoyed. You might stop going to movies, meetings, or events because you don’t want to use the restroom in the middle of an activity or have an accident. These lifestyle changes can lead to depression NIH external link or social anxiety NIH external link.
If you often feel depressed or anxious about living with bladder control problems, talk with a health care professional.
Intimacy problems
Some people may avoid intimacy because they worry they may leak urine during sex. Talk with a health care professional if your bladder control problems are getting in the way of your sex life. Gynecologists and urologists regularly talk with people about health problems and can offer solutions.
Related bladder symptoms and problems
If you have UI, you are more likely to have other bladder symptoms or problems, such as
- urinary frequency
- getting up from sleep to urinate, called nocturia
- difficulty urinating
- trouble emptying your bladder fully, called urinary retention
- dribbling urine after you think you’ve finished
When speaking about other symptoms you may have with UI, health care professionals may use the term LUTS, which stands for lower urinary tract symptoms.
Working with a health care professional to prevent and treat these related symptoms and problems is important for the health of your bladder and your overall health.
References
Symptoms & Causes
In this section:
- What are the symptoms of bladder control problems?
- When should I see a health care professional?
- What causes bladder control problems?
- What else causes bladder control problems in women?
- What else causes bladder control problems in men?
What are the symptoms of bladder control problems?

Signs and symptoms of urinary incontinence (UI) can include
- leaking urine during everyday activities, such as lifting, bending, coughing, or exercising
- being unable to hold in urine after feeling a sudden, strong urge to urinate
- leaking urine without any warning or urge
- being unable to reach a toilet in time
- wetting your bed during sleep
- leaking during sexual activity
When should I see a health care professional?
See a health care professional if you have symptoms of a bladder problem, such as trouble urinating, a loss of bladder control, waking to use the bathroom, pelvic pain, or leaking urine.
Bladder problems can affect your quality of life and cause other health problems. Your health care professional may be able to treat your UI by recommending lifestyle changes or a change in medicine.
Seek care right away
See a health care professional if you
- can’t pass urine or empty your bladder, which is a sign of urinary retention
- urinate too often—eight or more bathroom visits a day—also called frequency
- see blood in your urine, called hematuria
- have bladder infection symptoms, including painful urination
These symptoms can signal a serious health problem, including inflammation of the bladder, also called cystitis, or even bladder cancer NIH external link.
What causes bladder control problems?
Health changes and problems, including those with your nervous system, and lifestyle factors can cause or contribute to UI in women and men.
Health changes and problems
Health changes and problems that can lead to UI, include
- aging
- bladder infection
- constipation
- birth defects NIH external link
- blocked urinary tract—from a tumor or kidney stone
- chronic, or long-lasting, cough
- diabetes
- overweight or obesity
- genitourinary fistulas NIH external link
Some health problems can be short-term, like a urinary tract infection or constipation, and can cause temporary incontinence.
Nerve damage
Problems with the nervous system are common causes of UI. Nerves carry messages from the bladder to the brain to let it know when the bladder is full. Nerves also carry messages from the brain to the bladder, telling muscles either to tighten or release. The brain decides if it’s an acceptable time to urinate. Functional incontinence can occur when there is a problem getting the messages from your brain to a part of your urinary tract—usually the bladder, the sphincters, or both.
View full-sized image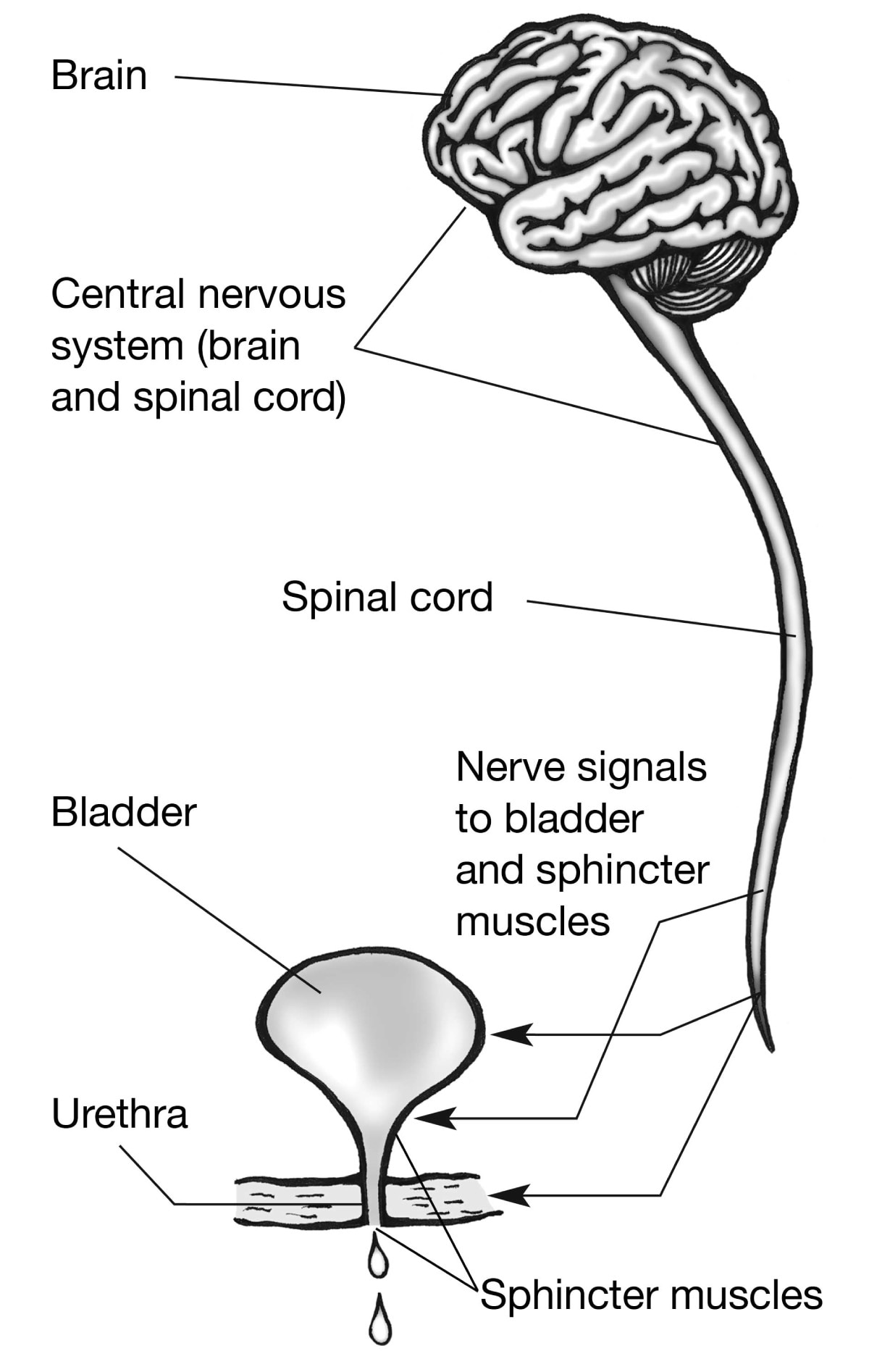 Nerves carry signals from your brain to your bladder and sphincter muscles.
Nerves carry signals from your brain to your bladder and sphincter muscles.
Bladder nerves and muscles can be damaged or affected by
- diabetes
- vaginal childbirth
- surgery for prostate cancer
- stroke
- Parkinson’s disease NIH external link
- multiple sclerosis NIH external link
- Alzheimer’s disease NIH external link
- brain or spinal cord injury
- anxiety NIH external link
- heavy metal poisoning
Triggers that may cause a sudden, strong urge to urinate can include drinking or touching water, hearing running water, or being in a cold environment, such as reaching into the freezer at the grocery store.
Lifestyle factors
Lifestyle factors that make women and men more likely to experience UI include
- eating habits, such as eating foods that cause constipation
- drinking habits, such as drinking alcohol or caffeinated or carbonated beverages
- certain medicines
- physical inactivity
- smoking
Temporary incontinence is usually a side effect of a medicine or short-term health condition. Temporary incontinence can also be a result of eating and drinking habits, including using alcohol or caffeine.
What else causes bladder control problems in women?
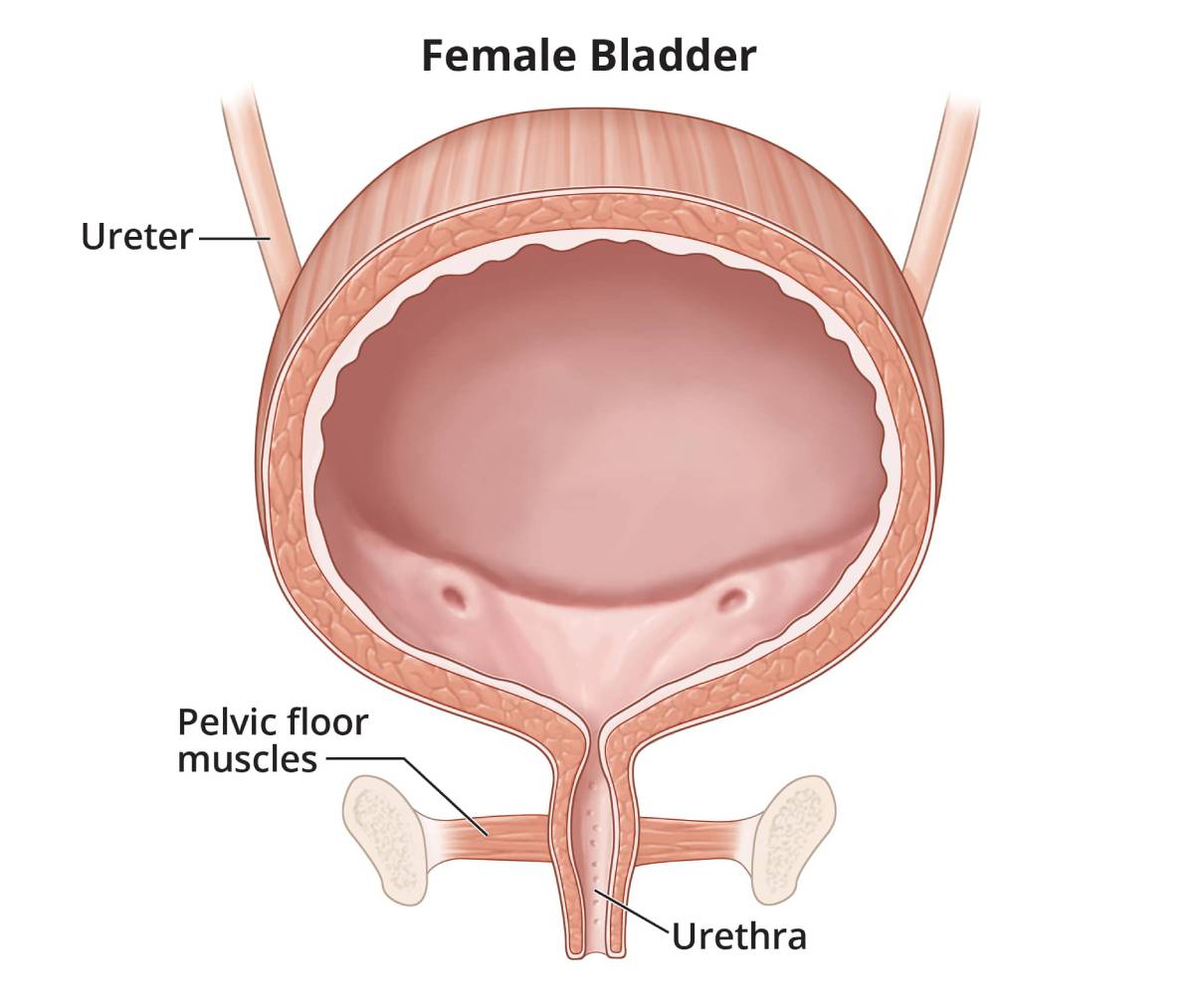
Certain life events and health problems can lead to stress incontinence in women by weakening the pelvic floor muscles
- pregnancy and childbirth
- trauma or injury, such as sexual assault
- pelvic organ prolapse NIH external link, such as a cystocele
- menopause NIH external link
Weak pelvic floor muscles can make it hard for your bladder to hold urine in during stress incontinence. Stress incontinence occurs when an action—coughing, sneezing, laughing, or physical activity—puts pressure on your bladder and causes urine to leak. A weak pelvic floor can also cause fecal incontinence, or bowel control problems.
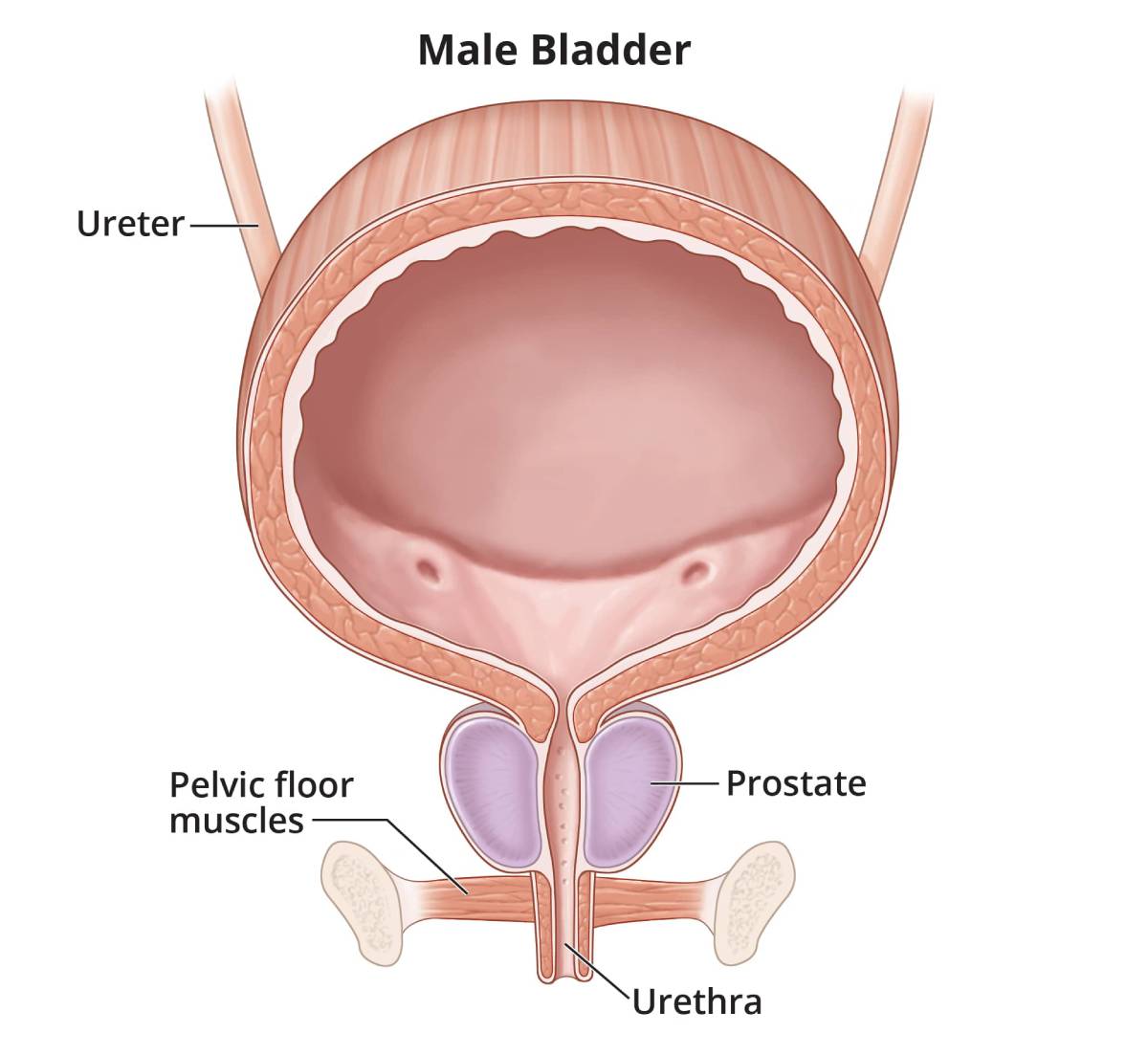
What else causes bladder control problems in men?
Men sometimes develop UI along with prostate problems.
Prostate problems
Men have a prostate gland that surrounds the opening of the bladder. The prostate gets bigger as a man grows older. When a man’s prostate gets too big but isn’t cancerous, he has a condition called prostate enlargement, or benign prostatic hyperplasia (BPH). Men with an enlarged prostate may have
- problems starting to urinate
- a slow urine stream
- problems fully emptying the bladder
Treatment for BPH can lead to stress incontinence, but it is usually temporary.
Men who have a history of radiation NIH external link or surgery for prostate cancer NIH external link may have short-term or long-term UI. Surgery NIH external link, radiation, or other prostate cancer treatments can lead to nerve damage, bladder spasms, or stress incontinence. Bladder control problems after prostate cancer treatment can get better over time.
Diagnosis
How do health care professionals find the cause of a bladder control problem?
A health care professional will ask about your family and medical history and give you a physical exam. The exam will look for medical problems that may lead to accidental urine loss, also called urinary incontinence (UI). You may be asked to cough while your bladder is full to see if you leak urine. This is called a stress test, and health care professionals use it to help diagnose stress incontinence.
 Even if you feel embarrassed, it’s important to talk with a health care professional if you’re having bladder control problems.
Even if you feel embarrassed, it’s important to talk with a health care professional if you’re having bladder control problems.Additionally, you may be asked to keep a bladder diary, and your health care professional may order labs and other diagnostic tests.
Bladder diary
A bladder diary (PDF, 487.59 KB) is a record of
- what, when, and how much you drink
- when you urinate and the amount you urinate
- how often you leak
- whether you feel a strong urge to go before a urine leak
- what you were doing when the leaks happened
You may want to keep a bladder diary for 2 to 3 days before seeing your health care professional. This helps your health care professional see patterns to narrow down the cause of your bladder control problems.
What tests do health care professionals use to help find the cause of a bladder control problem?
Your health care professional may order one or more tests to help find the cause of UI.
- Urinalysis NIH external link can test your urine for a bladder infection, a kidney problem, or diabetes.
- Blood tests NIH external link can show problems with how well your kidneys work or a chemical imbalance in your body.
- Urodynamic testing, including electromyography, looks at how well parts of the urinary tract—the bladder, urethra, and sphincters—are storing and releasing urine.
- Cystoscopy is a procedure that uses a cystoscope—a long, thin instrument—to look inside the urethra and bladder.
- Imaging tests NIH external link can be used to take pictures of the inside of the body, including the urinary tract and nervous system.
Treatment
Can I treat my bladder control problem myself?
Depending on the type of urinary incontinence (UI) you have, your health care professional may recommend steps you can take on your own to try to control your symptoms.
Make lifestyle changes
You may be able to reduce leaks by making lifestyle changes.
Drink the right amount of liquid at the right time
Ask your health care professional whether you should drink less liquid during the day. However, don’t limit liquids to the point of becoming dehydrated. Your health care professional can tell you how much and when to drink, based on your health, activities, and local climate.
To limit nighttime trips to the bathroom, you may want to stop drinking liquids a few hours before bedtime, but only if your health care professional suggests it. Limiting foods and drinks with caffeine, such as chocolate, tea, coffee, and carbonated beverages, may help reduce leaks. You should also limit alcoholic drinks, which can increase how much urine your body makes.
The amount of urine a person should make is different for everyone, based on how much liquid you drink, how much you sweat, how much liquid you lose by breathing, and the medicines you take.
Be physically active
Although you may not feel like being physically active when you have UI, regular physical activity is important for weight management and good overall health. Activities such as walking, swimming, biking, and dancing can improve your health. If you’re concerned about not having a bathroom nearby during physical activity, find a place with nearby restrooms, such as a shopping mall, community park, or local gym.

Keep a healthy weight
Your chances of developing UI and other diseases, such as diabetes, are higher if you’re overweight or have obesity. Losing weight can help you have fewer leaks, and avoiding weight gain may prevent UI. Studies suggest that as your body mass index (BMI) increases, you’re more likely to leak.4 If you’re overweight or have obesity, talk with your health care professional about how to lose weight.
Avoid constipation
Constipation can make urinary tract health worse and can lead to UI. Talk with your health care professional about drinking more liquids and eating enough fiber to avoid constipation. Health care professionals use medicines called anticholinergics, tricyclic antidepressants NIH external link, and beta-3 agonists NIH external link to treat UI, but they can cause constipation.
Stop smoking
If you smoke, get help to stop smoking External link. Quitting smoking at any age is good for your bladder health and overall health. Smoking raises your chances of developing stress incontinence, because smoking causes chronic, or long-lasting, coughing. You might improve your UI if you’re able to stop coughing.5
Smoking also causes most cases of bladder cancer NIH external link. Some people say smoking irritates their bladder.
Train your bladder
Bladder training is when you urinate on a schedule to reduce leaking. Your health care professional may use your bladder diary (PDF, 487.59 KB) to suggest you use the bathroom on a regular schedule, called timed voiding. Gradually lengthening the time between trips to the bathroom can help stretch your bladder so it can hold more urine. Record your daily bathroom habits so you and your health care professional can review your diary.
Do pelvic floor muscle exercises
Strong pelvic floor muscles hold in urine better than weak muscles. You can strengthen your pelvic floor muscles by doing Kegel exercises. These exercises involve tightening and relaxing the muscles that control urine flow. Researchers found that women who received pelvic floor muscle training had fewer leaks per day than women who didn’t receive training.6 You should not do pelvic floor exercises while you’re urinating.
Men can also benefit from pelvic floor muscle exercises. Strengthening these muscles may help a man leak urine less often, especially dribbling after urination.
A health care professional, such as a physical therapist trained in pelvic floor therapy, can help you get the most out of your Kegel exercises by helping you improve your core muscle strength. Your core includes your torso muscles, especially the lower back, pelvic floor muscles, and abdomen. These muscles keep your pelvis lined up with your spine, which helps with good posture and balance. Your physical therapist can show you how to do some exercises during daily activities, such as riding in a car or sitting at a desk.
You don’t need special equipment for Kegel exercises. However, if you are unsure whether you are doing the exercises correctly, you can learn how to perform Kegel exercises properly by using biofeedback, electrical stimulation, or both. Biofeedback uses special sensors to measure muscle contractions that control urination.
Control your urge to urinate
You may be able to control, or suppress, the strong urge to urinate, which is called urge or urgency suppression. With this type of bladder training, you can worry less about finding a bathroom in a hurry. Some people distract themselves to take their minds off needing to urinate. Other people find that long, relaxing breaths or holding still can help. Doing pelvic floor exercises to strengthen your pelvic floor also can help control the urge to urinate. Quick, strong squeezes of the pelvic floor muscles can help suppress urgency when it occurs, which may help you get to the toilet before you leak.
How can my health care professional treat my bladder control problem?

If lifestyle changes aren’t working for you, your health care professional may prescribe medicine, a medical device, a bulking agent, or—as a last resort—surgery to help treat UI.
Medicines
Urgency incontinence may be treated with one of the following medicines as a pill, liquid, or patch to relax your bladder
- anticholinergics
- beta-3 agonists
- tricyclic antidepressants
Health care professionals may use botulinum toxin A NIH external link, also known as Botox, to treat UI when other medicines or self-care treatments don’t work. Botox may be injected into your bladder. Injecting Botox into the bladder relaxes it, which makes more room for urine and lowers the chances of urine leaks.
In addition to anticholinergics, men with UI who have an enlarged prostate may also be prescribed
Medical devices
Catheter
Individuals with overflow incontinence may need to use a catheter to empty their bladder. Your health care professional will teach you how to use a catheter. Proper hygiene is important for catheter use and to avoid a bladder infection.
Pessary
Women may use a soft, plastic device called a pessary, which is inserted into the vagina for stress incontinence. The pessary presses against the wall of your vagina and the nearby urethra. The pressure helps hold up the urethra, so you have less leaking.
Another newer product to treat stress incontinence is a tampon-like disposable device that you can insert into your vagina for up to 12 hours at a time. The product expands to push up against your urethra to help decrease leaks.
Bulking agents
Gel or paste can be injected near your urinary sphincter to treat stress incontinence. The injected material bulks up the area around the urethra. The extra thickness helps close your bladder opening so you leak less.
Electrical nerve stimulation
If medicines and lifestyle changes don’t help your UI, your health care professional may suggest electrical nerve stimulation for urgency incontinence and other symptoms. Electrical nerve stimulation changes your bladder’s reflexes, using mild pulses of electricity to stimulate the nerves that control the bladder and sphincter muscles.
Surgery
Sling surgery
The most common surgery to treat stress incontinence in women is sling surgery. In sling surgery for women, a surgeon works through the vagina to insert a strip of material between the vagina and urethra. The surgeon may choose to use a synthetic mesh External link, a screen-like material that supports weakened or damaged tissue, or the surgeon may choose a biologic graft made from human or animal tissue.
Although sling surgery with synthetic mesh can be successful and safe, complications can occur in some women. Your health care professional can explain the risks and benefits of surgery for stress incontinence and what kind of results you can expect.
Stress incontinence in men can be treated with the male sling—a procedure in which mesh is placed under the urethra, lifting and supporting the urethra and sphincter muscles.
Artificial urinary sphincter
Stress incontinence in men can be treated by implanting an artificial urinary sphincter—a device that helps keep the urethra closed to prevent leaks.
Surgery to remove a blockage
Overflow incontinence caused by a blockage or a narrowed urethra can be treated with surgery to remove the blockage.
Bladder outlet obstruction may occur in men who have an enlarged prostate. When other treatments don’t work well enough, your health care professional may suggest surgery, including minimally invasive surgery, to remove enlarged prostate tissue or to widen the urethra.
Bladder enlargement, or bladder augmentation
If UI is caused by nerve damage, your health care professional may suggest surgery to make your bladder larger. This procedure may allow your bladder to store more urine but can make the bladder more difficult to empty, which may require you to use a catheter to empty your bladder.
 Try lifestyle changes to treat your bladder problem. If that doesn’t work, your health care professional may prescribe medicine, a medical device, or a bulking agent.
Try lifestyle changes to treat your bladder problem. If that doesn’t work, your health care professional may prescribe medicine, a medical device, or a bulking agent.
How can I cope with bladder control problems?
Protective products
Even after treatment, you may still leak urine from time to time. Certain products can help you cope with urine leaks
- Absorbent, washable incontinence underwear. You can use underwear lined with special fabric that absorbs urine.
- Waterproof underwear. Waterproof underwear can protect your clothes from getting wet.
- Adult incontinence briefs. You can wear disposable incontinence briefs that act like diapers to keep your clothes dry.
- Pads. You can wear disposable pads in your underwear to absorb leaking urine.
- Large disposable pads. You can use large pads to protect chairs and beds from urine.
- Special skin cleaners and creams. Special skin cleaners and creams may keep the skin around the urethra from getting irritated. Creams can help block urine from your skin.
- Urine deodorizing tablets. Talk with your health care professional about whether taking urine deodorizing tablets by mouth can make your urine smell less strong.
- External catheters. An external catheter, used by men, can collect urine from a man’s body and drain it into a bag that is attached to the thigh with a strap.
Emotional support
Bladder control problems are common, yet many people feel too embarrassed to talk about them. At the very least, talk with your health care professional about your bladder problems. Your health care professional can help you connect with a support group for people with similar problems.
Consider speaking with your family and friends about your UI. Your family and friends may make it easier for you to manage UI. In sharing your struggle, you may find that other people in your life have bladder problems as well.
References
Prevention
How can I prevent bladder control problems?
You can’t always prevent bladder control problems such as urinary incontinence (UI), but good habits can keep your bladder as healthy as possible.
Follow a healthy eating plan
Healthy eating External link may prevent factors that raise your chances of developing UI, such as obesity and diabetes. No direct scientific evidence links nutrition to making UI better or worse.
Many people find that alcohol; spicy foods; chocolate; artificial sweeteners; caffeinated, carbonated, and citrus beverages; and high-acid foods, such as citrus and tomatoes, may contribute to bladder irritation and inflammation, which can sometimes lead to UI. You may want to avoid these foods and drinks for a time to see if your symptoms improve. A registered dietitian can help you plan meals External link if you’re trying to avoid certain foods that make your UI worse.
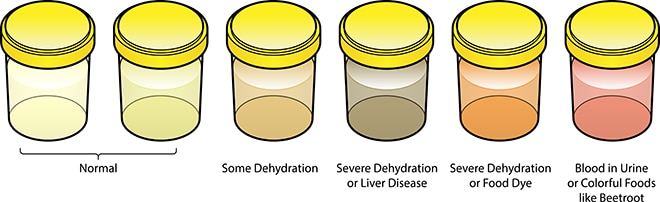
Drink enough liquids
Drink enough liquids so you need to urinate every few hours. Learn what’s normal for you and avoid becoming dehydrated. Your urine should be pale yellow if you are drinking enough liquids. Talk with your health care professional about how much liquid you should drink based on your size, activity level, and where you live. Water is best. However, if you have kidney failure or heart failure, you should not drink too much water.
Keep a healthy weight

If you’re overweight or have obesity, losing weight may improve your UI, and keeping a healthy weight may prevent UI. If you’re overweight, talk with your health care professional about how to lose weight by eating healthy and being physically active. Your chances of developing UI and other diseases and conditions, such as diabetes, increase if you have obesity. Managing obesity and diabetes may lessen UI, especially in women.7
Change your bathroom habits
Go to the bathroom when you need to go. Often, people hold their urine in because it’s not a convenient time to go to the bathroom. However, regularly holding urine in can wear out your bladder muscles. You’re also more likely to develop a bladder infection if you hold urine in. Bladder infections can cause UI.
Women should try to relax the muscles around their bladder when they urinate to make it easier to go. It’s best to sit on the toilet seat or in a full crouching squat. Hovering over a toilet seat to avoid touching it does not allow the muscles to fully relax, and urine may be left in the bladder. Take as much time as you need to urinate and fully empty your bladder.
Quit smoking
Quitting smoking External link at any age is good for your bladder health and overall health. Smoking raises your chances of developing stress incontinence, because smoking causes coughing. Smoking also causes most cases of bladder cancer NIH external link. Some people say smoking makes their bladder irritation worse.
Avoid constipation
Constipation can make urinary tract health worse and can lead to UI. To prevent constipation, eat plenty of high-fiber foods such as whole grains, vegetables, and fruits; drink enough water; and be physically active. Medicines that health care professionals use to treat UI, such as anticholinergics, have side effects that include constipation.
Do pelvic floor muscle exercises
Pelvic floor muscles help hold urine in the bladder. Pelvic floor exercises, also called Kegel exercises, can make those muscles stronger and help keep urine from leaking out when you laugh, cough, sneeze, or lift. Both men and women can benefit from pelvic floor muscle exercises.
References
Clinical Trials
The NIDDK conducts and supports clinical trials in many diseases and conditions, including urologic diseases. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for bladder control problems?
Clinical trials—and other types of clinical studies NIH external link—are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help health care professionals and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of bladder control problems, such as
- new and more effective ways to control urinary incontinence (UI)
- the use of biofeedback to control urgency incontinence
- the use of nerve stimulation to restore bladder function in individuals with neurologic injuries
Find out if clinical studies are right for you. NIH external link
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical studies for bladder control problems are looking for participants?
You can view a filtered list of clinical studies on bladder control problems that are open and recruiting at ClinicalTrials.gov NIH external link. You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the NIH does not review these studies and cannot ensure they are safe. Always talk with your health care professional before you participate in a clinical study.
How is NIDDK- and NIH-funded research advancing the understanding of bladder control problems?
The NIDDK and the NIH have supported many research projects to learn more about bladder control problems, including the Symptoms of Lower Urinary Tract Dysfunction Research Network (LURN) External link and the Prevention of Lower Urinary Tract Symptoms (PLUS) Research Consortium External link. The LURN and PLUS Research Consortium conduct research to advance our understanding of bladder control problems and to improve prevention and intervention strategies for bladder health.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
The NIDDK would like to thank:
Joseph A. Costa, D.O., University of Florida Health, Jacksonville, and Behzad Jazayeri, M.D., University of Florida, Jacksonville College of Medicine

