Hydronephrosis in Newborns
On this page:
- What is hydronephrosis in newborns?
- Does hydronephrosis have other names?
- How common is hydronephrosis in newborns?
- Who is more likely to have hydronephrosis?
- Is hydronephrosis a sign of a problem?
- What are the signs or symptoms of hydronephrosis in a newborn?
- What causes hydronephrosis in newborns?
- How do health care professionals diagnose hydronephrosis before an infant is born?
- How do health care professionals diagnose hydronephrosis in newborns?
- How do health care professionals treat hydronephrosis in newborns?
- Clinical Trials for Hydronephrosis in Newborns
What is hydronephrosis in newborns?
Hydronephrosis in newborns is enlargement, or dilation, of the renal pelvis—the basin in the central part of the kidney where urine collects. Hydronephrosis can occur in one or both kidneys. This condition is often diagnosed before birth during a prenatal ultrasound.
In some cases, hydronephrosis is mild and goes away on its own without treatment. In other cases, hydronephrosis may be a sign of a blockage in the urinary tract or reflux—or back up—of urine from the bladder to the kidney that needs treatment.
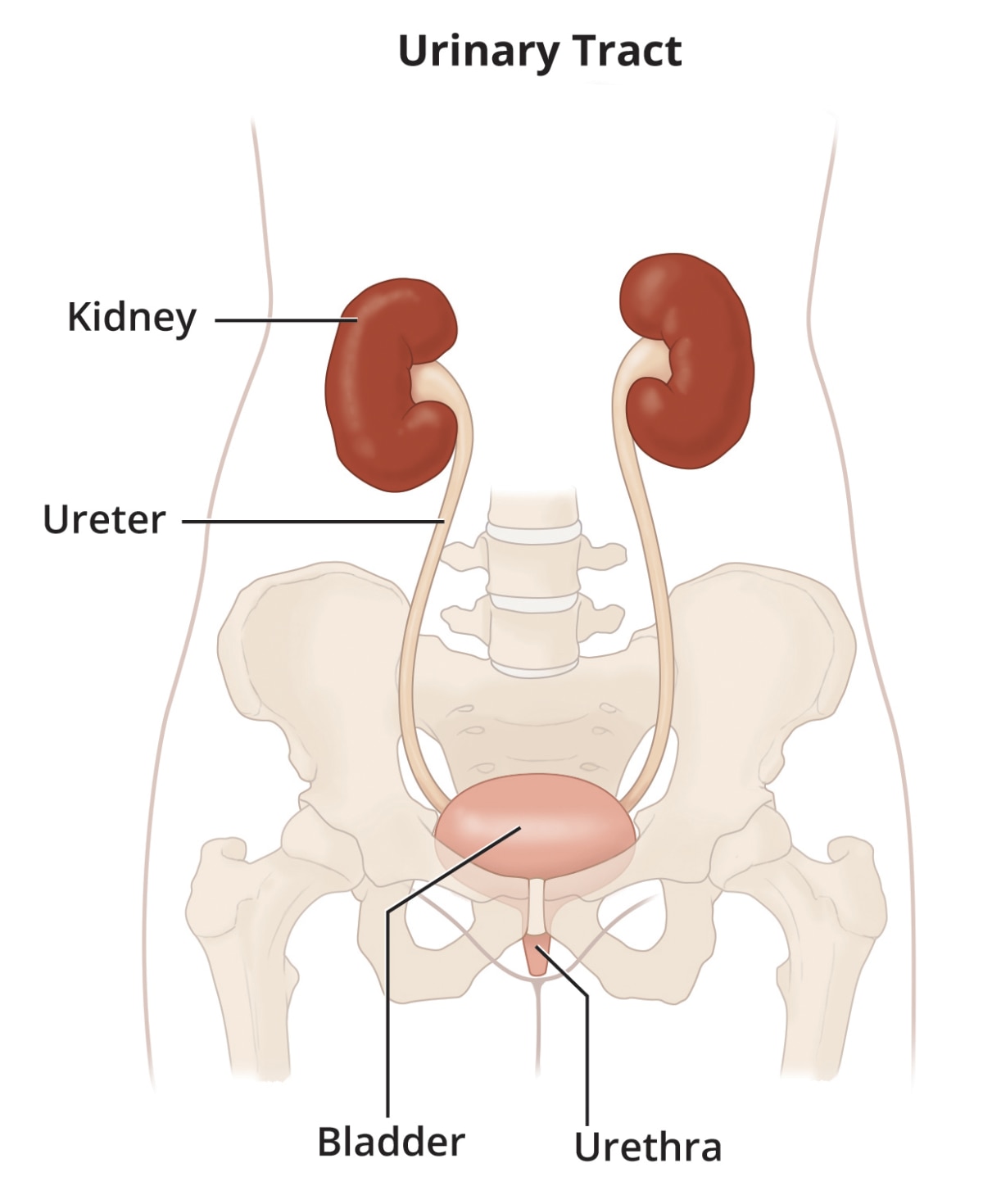
The urinary tract is the body’s drainage system for removing wastes and extra fluid. The urinary tract includes the kidneys, ureters, bladder, and urethra.
Does hydronephrosis have other names?
Hydronephrosis may be called other names, including
- antenatal, fetal, or prenatal hydronephrosis, when the condition is diagnosed before birth
- dilated or enlarged urinary tract
How common is hydronephrosis in newborns?
In 1 or 2 out of every 100 pregnancies, the fetus is diagnosed with hydronephrosis.1 In about half of these cases, the hydronephrosis goes away by the time the infant is born.2
Who is more likely to have hydronephrosis?
Males are about twice as likely as females to have hydronephrosis.3
Is hydronephrosis a sign of a problem?
If a fetus or newborn is found to have hydronephrosis, health care professionals will begin to examine how urine drains from the kidneys. The more severe hydronephrosis is, the more likely it is to be a sign of a blockage in the urinary tract or reflux of urine from the bladder to the kidney, which may need treatment. Early diagnosis and treatment of the blockage or reflux may help prevent complications or prevent complications from getting worse.
Normally, the fetus’s urine becomes part of the amniotic fluid that surrounds the fetus in the womb. In a fetus with severe hydronephrosis, too much urine may stay in the urinary tract, leading to low levels of amniotic fluid in the womb. Low levels of amniotic fluid can harm the fetus’s developing lungs.
After an infant is born, hydronephrosis may lead to complications such as urinary tract infections, kidney stones, and chronic kidney disease.
What are the signs or symptoms of hydronephrosis in a newborn?
Newborns with hydronephrosis often do not show signs. In some newborns, the abdomen may be swollen due to severe blockage of the urinary tract. In other cases, newborns with hydronephrosis may develop a urinary tract infection, which may cause signs or symptoms.
If your child has been diagnosed with hydronephrosis, talk with your child’s health care professional about appropriate evaluation and treatment options.
What causes hydronephrosis in newborns?
In some fetuses and newborns with hydronephrosis, health care professionals can’t find a cause, and the hydronephrosis goes away on its own. This is called transient hydronephrosis.
In other cases, hydronephrosis is caused by a blockage in the urinary tract or reflux of urine from the bladder to the kidney.
Transient hydronephrosis
Experts think that narrowing of part of the urinary tract during early development may cause transient hydronephrosis. The condition resolves as the urinary tract matures.
About half of fetuses diagnosed with hydronephrosis have transient hydronephrosis, and the condition goes away before the infant is born. In children who are born with hydronephrosis, the condition is sometimes transient and can go away on its own, usually by the time the child is age 3.2
Birth defects
Birth defects in the urinary tract may cause hydronephrosis. Even when birth defects are the cause, hydronephrosis may be mild and may improve as the child gets older. However, birth defects may also cause hydronephrosis that is severe or gets worse over time.
Ureter defects. Birth defects in the ureter that cause hydronephrosis include
- ureteropelvic junction (UPJ) obstruction, in which a blockage is present where the ureter joins the renal pelvis
- vesicoureteral reflux (VUR), in which urine flows backward, or refluxes, from the bladder to one or both ureters and sometimes to the kidneys
- other defects of the ureter or where the ureter joins the bladder, which may prevent the normal flow of urine from the kidneys to the bladder
Among all birth defects that cause hydronephrosis in fetuses and newborns, UPJ obstruction and VUR are most common.1
Lower urinary tract obstruction. In lower urinary tract obstruction, also called bladder outlet obstruction, a blockage is present in the urethra or where the bladder joins the urethra. Birth defects that cause lower urinary tract obstruction include posterior urethral valves, which are abnormal folds of tissue that block the urethra. Posterior urethral valves only occur in males. Because lower urinary tract obstruction blocks urine flow from both kidneys, it is more urgent for doctors to examine lower urinary tract obstruction than blockage or reflux in a ureter.
Defects in the urinary tract and other parts of the body. Some infants with hydronephrosis have birth defects in the urinary tract and in other parts of their body. For example, prune belly syndrome is a group of birth defects that includes poorly developed abdominal muscles, undescended testicles, and urinary tract defects.
Birth defects that affect the spinal cord, such as spina bifida, can affect the nerves that control the urinary tract and cause urinary retention. Urine retained in the bladder may flow backward into the ureters and kidneys, causing hydronephrosis.
How do health care professionals diagnose hydronephrosis before an infant is born?
Health care professionals can diagnose hydronephrosis before an infant is born during a prenatal ultrasound. Ultrasound bounces safe, painless sound waves off the fetus’s organs to create an image of their structure. An ultrasound can show that parts of the urinary tract are enlarged due to hydronephrosis.
Ultrasounds during pregnancy are part of routine prenatal testing. If a fetus is diagnosed with hydronephrosis, health care professionals may recommend additional ultrasounds to find out if hydronephrosis gets worse or improves over time. Health care professionals may also use ultrasounds or other prenatal tests to try to find the cause of hydronephrosis or check for other health problems.
How do health care professionals diagnose hydronephrosis in newborns?
Health care professionals use a newborn’s medical history, a physical exam, and imaging tests to diagnose hydronephrosis.
Medical history
Health care professionals use the results of prenatal ultrasounds and other prenatal tests to determine what kind of testing or treatment infants will need after birth.
Physical exam
During a physical exam, a health care professional will check for a lump or mass in the abdomen, which could be a sign of an enlarged kidney or bladder. A health care professional will also check for signs of birth defects in other parts of the body.
Imaging tests
Health care professionals may use urinary tract imaging tests to diagnose and find the cause of hydronephrosis. Imaging tests may include
- ultrasound, which uses sound waves to view the child’s urinary tract
- voiding cystourethrogram, which uses x-rays to show how urine flows through the bladder and urethra
- radionuclide scan, which creates images of the urinary tract as a radioactive substance passes through
How do health care professionals treat hydronephrosis in newborns?
Treatment of hydronephrosis in newborns will depend on
- how severe the condition is
- whether one or both kidneys are affected
- what is causing the hydronephrosis
Treatments may include watchful waiting, preventing and treating urinary tract infections, and surgery.
Watchful waiting
If hydronephrosis in a newborn is not severe and not likely to damage the kidneys, health care professionals may recommend watchful waiting. Health care professionals will perform tests from time to time to see if hydronephrosis changes or causes kidney damage as the infant gets older.
Hydronephrosis may improve or go away over time. However, if hydronephrosis gets worse or causes complications, a health care professional may recommend surgery.

Preventing and treating urinary tract infections
In some cases, health care professionals may prescribe antibiotics to help prevent urinary tract infections in infants and children with hydronephrosis. If a child develops a urinary tract infection, antibiotics are also used to treat the infection.
Research suggests that, in male infants with hydronephrosis, circumcision may lower the chance of getting urinary tract infections.4
Surgery
If hydronephrosis is severe or gets worse over time, health care professionals may recommend surgery. Surgery can improve the flow of urine and lower the chance of complications or keep complications from getting worse.
Health care professionals rarely perform surgery to treat hydronephrosis in a fetus while it’s still in the womb. Fetal surgery carries many risks, so it is performed only in special cases.
Clinical Trials for Hydronephrosis in Newborns
The NIDDK conducts and supports clinical trials in many diseases and conditions, including urologic diseases. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials and what role do children play in research?
Clinical trials are research studies involving people of all ages. Clinical trials look at safe and effective new ways to prevent, detect, or treat disease. Researchers also use clinical trials to look at other aspects of care, such as improving quality of life. Research involving children helps scientists
- identify care that is best for a child
- find the best dose of medicines
- find treatments for conditions that only affect children
- treat conditions that behave differently in children
- understand how treatment affects a growing child’s body
Find out more about clinical trials and children.
What clinical trials are open?
Clinical trials that are currently open and are recruiting can be viewed at
ClinicalTrials.gov.
References
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
The NIDDK would like to thank:
Robert L. Chevalier, M.D., University of Virginia School of Medicine

